NMIN
projects
Theme I: Targeted Drug Delivery
Neutrophil encapsulation platform for targeted drug delivery
Theme I: Targeted Drug Delivery
Host institution: University of Toronto
To achieve targeted, cell-mediated drug delivery, this project proposes to hijack human white blood cells (neutrophils) and use them to deliver drugs. In vitro generated neutrophils, loaded with liposomes containing rational combinations of therapeutics, will naturally migrate to sites of disease characterized by inflammation, leading to localized drug delivery and reduced systemic toxicities.
Through collaboration with CCRM (Centre for Commercialization of Regenerative Medicine), our project team can generate large numbers of human neutrophils
ex vivo, which we have demonstrated can be successfully loaded with liposomes.
This proof-of-concept project application proposes to assess the clinical potential of our approach by optimizing the loading of liposomes into neutrophils, assessment of drug release and stability of neutrophils loaded with drug-containing liposomes, assessing drug release and stability of neutrophils loaded with drug containing liposomes, and testing the in vivo distribution and targeting ability of neutrophils in relevant animal models. As an initial indication, this project will target glioblastoma (GBM), a devastating malignancy with a five-year survival rate of less than 5%.
Future iterations of this technology can involve genetic engineering of cells with disease targeting moieties. Thus, this project will advance a new therapeutic modality to improve outcomes for patients in need, while also developing a platform technology where different therapeutic compounds of interest can be loaded into cells to target a variety of indications.

PI: Christine Allen
Collaborators:
Mitchell Cairo (New York Medical College); Robert Hancock (UBC); Anne Marinier (Institute for Research in Immunology and Cancer); John Marshall (University Health Network); Sheila Singh (McMaster University); Peter Zandstra (UBC)
Partners:Amplitude Ventures, CCRM, IRICoR, Perkin Elmer
Status:Active – funding cycle: 2019-2021
Development of the Metaplex immuno-oncology platform
Theme I: Targeted Drug Delivery
Host institution: University of British Columbia
Current cancer immune-therapies rely on antibodies or engineered cells targeting tumour-specific targets. Although they are highly successful in small populations
of patients with specific cancer types, these treatments
are complicated to implement and very costly.
Our research program aims to overcome these problems by developing treatments using drug-like molecules to effectively induce a phenomenon known as immunogenic cell death (ICD). The arising treatments should be applicable to a broad range of cancer types, but we are focused on development of intra-tumour injections for treatment of relapsed and refractory cervical cancer.
ICD is a process where dying cancer cells generate specific signals called DAMPs (damage-associated molecular patterns) to stimulate anticancer immunity. ICD is a promising approach to manage aggressive cancers due to its potential to supercharge the patient’s own immune system to recognize the patients own cancer. The immune system, if activated appropriately, will attack the cancer regardless of where it is located and regardless of how heterogeneous the cancer site may be. This treatment should also generate immunological memory, “vaccinating” the patient against future relapses.Our research team has discovered that copper can boost ICD effects.
This project will use the proprietary Metaplex technology to prepare combinations of candidate ICD-inducing compounds and copper in liposomes. This technology will facilitate the development of clinically relevant, novel treatments that would otherwise not be suitable for pharmacological development.
See the presentation and poster by Kent Chen on this project: The Metaplex Technology: A solution to the development of poorly soluble metal-binding small molecules

PI: Marcel Bally
Co-PIs:
Michael Abrams (Cuprous); Brad Nelson (BC Cancer & Cuprous); Ada Leung (Cuprous)
Partners:
BC Cancer, Cuprous, Faculty of Pharmaceutical Sciences (UBC); HATCH Accelerator (UBC), IRAP, Mitacs, NRC
Status:Active – funding cycle: 2019-2021
Triggered release of anticancer drugs from lipid nanoparticles
Theme I: Targeted Drug Delivery
Host institution: University of British Columbia
This project is aimed at developing lipid nanoparticle (LNP) systems containing anticancer drugs that will release their drug cargo specifically in target tumour tissue in response to an
external stimulus.
Our approach will entrap drug in long-circulating LNPs that also contain an agent that responds to external pulsed laser light or
intense oscillating magnetic fields.
Focused and sustained application of these external actuating factors to target tissue will then result in local drug release
that is sustained over hours or longer, resulting in dramatically
improved drug delivery to where
it is needed and associated improvements in therapy.
This project aims to identify methods of stimulating release from novel LNPs and to increase the amount of anticancer drug released at the target site by at
least tenfold, while also
reducing overall drug toxicity. It is expected that this improvement will result in curative therapies for many solid tumours.

PI: Pieter Cullis
Co-PIs:
Michel Meunier (Polytechnique Montréal); Lorne Whitehead (UBC)
Status:Active – funding cycle: 2019-2021
Nanoparticle formulations for anti-inflammatory IDR peptides
Theme I: Targeted Drug Delivery
Host institution: University of British Columbia
Inflammatory lung diseases including asthma, COPD, cystic fibrosis, and bronchiectasis are major causes of disability and eventual loss of life, accounting for 9.5 million deaths worldwide in 2008, one-sixth of the global total. Similarly, inflammatory skin conditions are a major cause of medical issues.
We have devised a series of peptides that have superb anti-inflammatory activity in animal models (including asthma, skin inflammation, bronchiectasis etc.) and work by mechanisms that are novel when compared to current anti-inflammatory agents—such as non-steroidal anti-inflammatories, to which patients can become tolerant over time.
To enable clinical trials of these peptides we must provide formulations that allow us to deliver them to optimize activity, suppress aggregation, and reduce toxicity and lability to enzymes (proteases) that destroy peptides, so as to enable the use of minimal doses of these molecules.
In this project, two major approaches will be pursued based on our experiences and research to date; namely, the use of lipids built into small units termed liposomal nanoparticles, and the use of variants of poly(lactic-co-glycolic acid) (PLGA), a polymer which has been used in a host of FDA-approved therapies due to its biodegradability and biocompatibility. The formulated peptides will be tested in relevant inflammation models that mimic human disease.

PI: Robert Hancock
Co-Investigators:
Azita Haddadi (University of Saskatchewan); Andrew Halayko (University of Manitoba); Sarah Hedtrich (UBC); Neeloffer Mookherjee (University of Manitoba)
Collaborator:
Pieter Cullis (UBC)
Partners:
ABT Innovations Inc., CIHR, Cystic Fibrosis Canada, Faculty of Science (UBC), Killam (UBC), MSFHR
Status:Active – funding cycle: 2019-2021
Nano-delivery of novel inhibitors of DNA repair for enhanced therapy in head & neck cancer
Theme I: Targeted Drug Delivery
Host institution: University of Alberta
Treatment of cancer often involves radiation therapy (RT), which works by damaging DNA. However, cancer cells have a robust DNA repair capacity. Inhibition of DNA repair enzymes can make cancer cells more sensitive to RT, increase cancer cell death and reduce the chance of cancer reoccurrence after treatment; however, they may act similarly on normal cells, leading to intolerable toxicities in patients.
Our team has recently developed novel small molecule inhibitors of a DNA repair enzyme—polynucleotide kinase/phosphatase (PNKP)—that have been shown to sensitize head and neck, lung, breast and
colorectal cancer cells to ionizing radiation. In this project, we propose to use nano-delivery systems encapsulating lead PNKP inhibitors, in order to: reduce their distribution and side effects in normal tissues; enhance tumor access to PNKP inhibitors; and, as a result, potentiate their
anti-cancer effects in combination with RT.
In the project, we will use these delivery systems in the treatment of head and neck cancer, particularly where the disease is in a locally advanced stage. The research aims to: benefit clinical outcomes in the management of head and neck cancer; expedite the translation to the clinic of Canadian-made novel inhibitors (PNKP) as new anti-cancer drugs; and open a new avenue for the use of nano-carriers in the drug development process.
See the presentation and poster by Forugh Sanaee on this project: Pharmacokinetics of Nano versus Conventional Formulations of A83B4C63, a Novel Inhibitor of DNA Repair in Rat

Co-PIs:
Quincy Chu (Cross Cancer Institute); Dennis Hall (University of Alberta); Michael Weinfeld (Cross Cancer Institute)
Collaborator:
Pieter Cullis (UBC)
Partners:
Alberta Cancer Foundation; Cross Cancer Institute; Meros Polymers; University of Alberta
Status:
Active – funding cycle: 2019-2022
Targeting myeloid leukemia with nanomedicines
Theme I: Targeted Drug Delivery
Host institution: University of British Columbia
Acute myeloid leukemia (AML) is a significant unmet medical need for which novel therapies are required. We have identified the histone methyltransferase
G9a/
EHMT2 as a novel type of modifier of tumoral activity. While drugs capable of inhibiting G9a in vivo have been developed, their administration triggers acute seizures and are too toxic to be used in vivo.
In this project, we propose to formulate G9a inhibitors as liposomal nanoparticles to prevent their toxic effects and enable their use in preclinical models. Our preliminary results indicate that encapsulation of a small molecule G9a inhibitor, UNC0642, in liposomes has the potential to prevent most of its toxic effects, while still impairing the ability of leukemic cells to grow in vitro.
With our
commercial partner, Integrated Nanotheraputics, who will supply the drug formulations to be tested, we will assess the safety and efficacy of this nanomedicine in vivo, in leukemic animals. Should we be successful, this drug would represent another weapon in the fight against AML, and as it targets a novel type of cancer-related pathway, it is likely to be used in combination therapies. This would lead to significant commercial opportunities for this specific formulation, but also support the notion that liposomal encapsulation can be used to improve drug efficacy and limit toxicity.
PI: Fabio Rossi
Co-PI:
Pieter Cullis (UBC)
Collaborator:
Aly Karsan (UBC)
Status:Active – funding cycle: 2019-2021
Targeting the NLRP3 inflammasome with lipid nanoparticles for the treatment of type 2 diabetes
Theme I: Targeted Drug Delivery
Host institution: University of British Columbia
This project proposes a new nanomedicine approach to treat type 2 diabetes, a disease associated with obesity and affecting millions of Canadians.
A major problem in current diabetes therapy is that no drug resolves the underlying inflammation in diabetic patients. We aim to develop a new nanomedicine for type 2 diabetes (T2D) that targets a major inflammatory pathway that is overactive in people with diabetes. We will use lipid nanoparticles (LNP), a clinically relevant drug delivery system, customized to carry anti-inflammatory drugs to macrophages, while limiting drug exposure in other cell types.
Chemists and LNP specialists on the team will generate and test
LNP to produce the best nanoparticle for delivering a drug to macrophages that shuts down an enzyme (called the NLRP3 inflammasome) that is essential for the production of toxic cytokines by macrophages. Our diabetes and immunology specialists will test the best LNP inhibitor in mouse models of diabetes and obesity, and measure the anti-inflammatory and anti-diabetic effects.
With close to half a billion people
worldwide suffering from T2D, a new cell-specific treatment has the potential to have a tremendous impact on global health and the economy. This project will also develop a new nanomedicine technology that can be applied to numerous other inflammatory and autoimmune diseases, potentially providing benefit to the research and medical community for development of additional nanomedicines that target the immune system.

PI: Bruce Verchere
Co-PIs:
Marco Ciufolini (UBC), Pieter Cullis (UBC)
Collaborators:Chris Tam (Integrated Nanotherapeutics)
Partners:BC Diabetes Research; Integrated Nanotherapeutics
Status:Active – funding cycle: 2019-2021
Lipidic nanoparticle formulation of a triple adjuvant for intranasal vaccines
Theme I: Targeted Drug Delivery
Host institution: University of Saskatchewan
We are developing a novel lipid nanoparticle formulation of a triple (three-component) adjuvant to be used for intranasal administration of vaccines for flu and whooping cough (pertussis).
The triple adjuvant is comprised of a peptide, RNA and a polymer that the immune system recognizes
as pathogen signals. Early-stage research has already established the effectiveness of the triple adjuvant for both flu and pertussis. This project uses novel lipid nanotechnology to improve its effect by the intranasal route. This strategy will expand the range of those who can be vaccinated as well as generating a more effective immune response (both mucosal and systemic), in addition to being less invasive than an injection. The physical properties of the lipid nanoparticle formulation help it reach the immune cells and provide additional stimulation.
Prior work shows that the lipid nanoparticle adjuvant formulation works well in animals using a model peptide intranasal vaccine. The proposed research will combine the lipid nanoparticle formulation with either inactivated flu virus or with antigens from the whooping cough bacteria (pertussis antigens), followed by intranasal administration to mice.
Outcomes will include evaluating the immune response to the vaccines such as antibodies and other biological immune mediators. We will also look at how the animals respond to a challenge with the infectious agent after vaccination, such as whether they get sick and how their immune system responds. The whooping cough vaccine will also be tested in newborn pigs to see if they can be protected from infection by the vaccine. The health of the nasal tissue and general health of the vaccinated animals will be evaluated as well.
See the presentation and poster by Noorjahan Aibani on this project: Design and in-vivo evaluation of lipid nanoparticles with a triple adjuvant to achieve enhanced immunity against Bordetella pertussis

PI: Ellen Wasan
Co-PIs:
Volker Gerdts (University of Saskatchewan), Yan Zhou (University of Saskatchewan)
Co-Investigators:
Robert Hancock (UBC), Kishor Wasan (University of Saskatchewan)
Partners:
VIDO-InterVac (University of Saskatchewan)
Status:
Active – funding cycle: 2019-2021
SI: Development of an aerosolized liposomal hydroxychloroquine for treating COVID-19 patients entering hospitals
Theme I: Targeted Drug Delivery
Host institution: University of British Columbia
Hydroxychloroquine (HCQ) is known to have anti-viral activity, but current clinical trials in patients with COVID-19 have indicated that the oral doses being given are not sufficient to elicit significant benefits. Clinical studies that have used HCQ doses considerably higher than the currently approved dose have resulted in deaths, and the use of high dose HCQ has been halted.
To address the potential for HCQ to be effective, Dr. Bally and Cuprous Pharmaceuticals Inc. (CPI) are developing an aerosolized liposomal formulation of HCQ that will increase the dose of HCQ in the lung and increase exposure time in this tissue while reducing the toxicity associated with HCQ use. The goal of this strategic initiative is to demonstrate its utility in vivo by showing increased drug exposure in the lung and reduced toxicity.

PI: Marcel Bally
Co-PIs:
Michael Abrams (Cuprous Pharmaceuticals), Ada Leung (Cuprous Pharmaceuticals), Tom Redelmeier (Cuprous Pharmaceuticals)
Collaborators:
Simon Authier (Cuprous Pharmaceuticals), Jim Blanshard (Cuprous Pharmaceuticals), Ghania Chikh (Cuprous Pharmaceuticals), Francis Dayton (Cuprous Pharmaceuticals), Igor Gonda (Cuprous Pharmaceuticals)
Partners:
Cuprous Pharmaceuticals
Status:
Complete – funding cycle: 2020-2021
Development of a targeted FAST-LNP formulation of cabazitaxel to improve efficacy and safety for prostate cancer treatment
Theme I: Targeted Drug Delivery
Host institution: University of Alberta
In this project, we propose to encapsulate the small molecule cabazitaxel in FAST-liposomes and assess the incorporation of ligand-directed targeting to cancer-specific receptors to improve efficacy and safety.
Taxane chemotherapies such as Cabazitaxel are currently approved for several solid tumours including prostate cancer, and this project will seek to improve their side-effect profile to further improve efficacy.
Successful implementation of the outputs of this project will have significant positive academic, social and economic impacts. Industry partners including Entos Pharmaceuticals, OncoSenX, Precision Nanosystems; academic partners such as the University of Alberta, the Alberta Prostate Cancer Research Initiative (APCaRI), the University of British Columbia, and the NMIN Network; and healthcare and patient stakeholders will benefit from the development of a well-tolerated, non-immunogenic, targeted delivery platform for oncology chemotherapy drugs such as cabazitaxel to prostate, breast and pancreatic cancers.

PI: John D. Lewis
Co-Investigators:
Roy Duncan (Dalhousie University)
Collaborators:Arun Raturi (Entos Pharmaceuticals), Michael Kolinski (University of Alberta), Adrian Fairey (University of Alberta)
Partners:
APCaRI, Entos Pharmaceuticals, OncoSenX, Precision Nanosystems, Sanofi Genzyme
Status:
Active – funding cycle: 2020-2022
Lipid Nanoparticle-mediated Immunotherapy for Pseudomyxoma Peritonei
Theme I: Targeted Drug Delivery
Host institution: University of British Columbia
Pseudomyxoma peritonei (PMP), also called jelly belly, is characterized by tumours spreading into the abdomen and forming jelly deposits. PMP is usually discovered at late stages and the 5-year survival rate of high-grade PMP is only 37.7%. The standard treatment is the combination of surgical removal with heated chemotherapy instilled into the abdomen, an aggressive treatment associated with significant complications in ~25% of the patients.
This project will develop a new treatment that will "wake up" the immune cells in the abdomen specifically to kill the spread cancers. This immune-activating effect will be localized in the abdomen without global stimulation of the immune system in the patient, and thus will be effective but cause little toxicity.
Our strategy is to develop a technology that can localize an immune-boosting drug in the abdomen, without the drug being absorbed into the blood stream to induce non-specific side effects.
This technology will also facilitate tumour antigen recognition by the immune cells in the abdomen, promoting specific killing of PMP. We will use non-human models to study how the targeted immune booster interacts with, and activates, the abdominal immune cells to clear PMP cells. The preliminary safety of the therapy will also be determined.
PI: Shyh-Dar Li
Collaborators:Sarah Hedtrich (UBC), Gregor Reid (UBC), Karla Williams (UBC)
Partners:
Appendix Cancer / Pseudomyxoma Peritonei Research Foundation
Status:
Active – funding cycle: 2020-2022
SI: Unlocking the full potential of cancer therapy
Theme I: Targeted Drug Delivery
Host institution: University of Victoria
The objective of this Strategic Initiative is to develop a novel strategy to enhance the benefits of radiotherapy (RT) by introducing two agents that could produce synergistic therapeutic effects during RTO. The PI’s most recent work shows that gold nanoparticles (GNPs), in combination with the anticancer drug docetaxel (DTX), produce synergistic therapeutic effect in breast and cervical cancers. Therefore, this team proposes to optimize the current RT protocol by using a triple combination of DTX, RT, and GNPs to treat pancreatic cancer.
Further, most of the current research is only focused on tumor cells. However, the tumor microenvironment also consists of fibroblast (FB) cells and cancer associated fibroblast cells (CAFs). FBs suppress tumor growth while CAFs promote tumor growth. Therefore, development of any targeted therapeutic approach should at least consider all three cell types. This team has been fortunate to receive CAFs and FBs (generated from pancreatic cancer patients) from the GI Biobank at Vancouver General Hospital, for this proposed project. This team has chosen MIA PaCa-2 as their standard pancreatic tumor cell line.

PI: Devika Chithrani
Co-PIs:Wayne Beckham (BC Cancer)
Co-Investigators:Abraham Alexander (BC Cancer), Daniel Renouf (BC Cancer), Chris Tam (Integrated Nanotherapeutics Inc.)
Partners:
BC Cancer, Integrated Nanotherapeutics Inc., Pancreatic Centre BC
Status:
Active – funding cycle: 2021-2022
SI: Preclinical regulatory plan for CounterFlow-Gauze, a non-compressible hemorrhage control dressing
Theme I: Targeted Drug Delivery
Host institution: University of British Columbia
This KTEE strategic initiative will further the advancement toward commercialization—lead by the spin-off company CoMotion Drug Delivery Systems Inc. (“CoMotion”)—of CounterFlow-Gauze: a gauze which contains self-propelling nanopores CaCO3 microparticles that can adsorb therapeutics. Specifically, this SI will underwrite the costs of sub-contracting a provider of regulatory guidance, to prepare Request for Designation (RFD) and pre-Investigational New Drug (IND) applications to the FDA.
CounterFlow-Gauze will compete with other non-absorbable hemostatic dressings, such as Combat Gauze, HemCon ChitoGauze, Celox, and XStat, for pre-hospital treatment of severe bleeding and non-compressible junctional bleeding for civilian and military settings. Preclinical studies that compared CounterFlow-Gauze head-to-head with one of these hemostatic products showed CounterFlow-Gauze is more effective.
Collaborator:
James Baylis (CoMotion)
Partners:
CoMotion Drug Delivery Systems Inc., Intertek Health Sciences Inc.
Status:
Active – funding cycle: 2021-2022
SI: NMIN Theme 1 Research & KTEE Accelerator
Theme I: Targeted Drug Delivery
Host institution: University of British Columbia
This KTEE strategic initiative will be implemented to maximize the translation and awareness of the knowledge/commercialization outputs of NMIN's Theme 1 (Targeted Drug Delivery) research projects.
A Research Accelerator/KT Specialist will be embedded within Theme 1 to work with the Research Leads, PIs, and NMIN Administrative Centre. This Research Accelerator/KT Specialist will: i) increase awareness, dissemination, and utilization of Theme 1 knowledge products (within NMIN and externally); ii) accelerate the commercialization potential of research results within Theme 1; and iii) enhance research management and knowledge mobilization expertise within NMIN Theme 1 and Network.
Nanoparticle-encapsulated PARPi and ATRi Combination Therapy for the Treatment of Ovarian Cancer
Theme I: Targeted Drug Delivery
Host institution: University of Toronto
The majority of women with ovarian cancer (OC) are diagnosed at an advanced stage, when the disease has spread beyond the ovaries. At this stage, the survival rate is significantly lower with limited effective treatment options.
In this project, to treat these patients we are proposing a new therapy involving a combination of two drugs, combined at specific amounts, and packaged into nanoparticles. These nanoparticles ensure that the drugs are delivered to the tumour site and are released at the specific ratios optimised to kill the cancer cells.
This research project brings together over 15 years of nanoparticle and drug combination research in the Allen Lab with Jazz Pharmaceuticals, a global biopharmaceutical company with extensive experience in the oncology space. The combined complementary experience of the Allen Lab and key members of Jazz Pharmaceuticals will expedite the preclinical development of this therapy and increase the likelihood of translation into the clinic.
PI: Christine Allen
Collaborators:
Robert Hauptschein (Jazz Pharmaceuticals); Paul Tardi (Jazz Pharmaceuticals)
Partners:Jazz Pharmaceuticals
Status:Active – funding cycle: 2021-2023
Theme II: Gene Therapy
GeneCure: Application of lipid nanoparticle technology to gene therapies in a variety of tissues
Theme II: Gene Therapy
Host institution: University of British Columbia
Genetic disorders, cancer, and infectious diseases affect millions of people around the globe, representing a considerable public health burden. Current therapeutic strategies have proven ineffective and expensive. Translating new small molecule drugs from drug discovery to the clinic is challenging; indeed, only 1 out of 10,000 small molecule drugs tested during development will make it to the clinic.
The advent of gene therapies
enabled by nanoparticulate delivery systems such as lipid nanoparticles (LNP) is a revolutionary development
that is making gene therapy
a real and immediate possibility
to treat all hereditary diseases. Further, LNPs encapsulating RNA- or DNA-based drugs are potentially now able to treat or even cure other
high-burden human diseases by silencing pathogenic genes, expressing therapeutic proteins, or correcting genetic defects. However, LNPs employed for gene therapy are currently optimized primarily for liver (hepatocyte) targets, limiting the number of potential disease indications
The GeneCure project will develop and optimize new LNP
systems that can access other target tissues in vivo. The GeneCure research program will
thus bring considerable incremental value by extending
in vivo gene therapy applications to a large variety of extra-hepatic tissues.

PI: Pieter Cullis
Co-Investigator:
Dominik Witzigmann (UBC)
Collaborators:
Jan Dutz (UBC), Marianna Foldvari (University of Waterloo), Kenneth Harder (UBC), Sarah Hedtrich, Christian Kastrup (Michael Smith Laboratories), Aneal Khan (University of Calgary), Brian MacVicar (UBC), Michel Meunier (Polytechnique Montreal), Robert Molday (UBC), Victor Rafuse (Dalhousie University), Colin Ross (UBC), Fabio Rossi (UBC), Molly Shoichet (University of Toronto), Terrance Snutch (UBC), Peter Zandstra (Michael Smith Laboratories)
Partners:
Integrated DNA Technologies
Status:
Active – funding cycle: 2019-2021
A multiomics screen to identify phagocyte-specific LNPs for immunotherapy
Theme II: Gene Therapy
Host institution: University of British Columbia
Current Immunotherapies—therapies to rejuvenate the immune system such as immune checkpoint blockade—can enhance the immune response against cancer, and, in some cases, is curative. However, many cancers do not respond to currently available immunotherapies. There is a pressing need to develop complementary immune regulatory strategies to improve current immunotherapies and increase the number of cancer types responsive to this form of treatment.
This proposal describes the development of a new immunotherapy strategy, using nanoparticles to deliver nucleic acids to specific immune cells, in order to reactivate them in a cancer setting.
There is a vast array of nanoparticle types (formulations) available, which differ with respect to the cells they home to in the body, and how well they deliver their nucleic acid cargo once inside cells. We will first establish a screen to determine which particular nanoparticle formulations best target and deliver nucleic acids to different types of immune cells. Next, we will test the ability of the lead nanoparticle formulations to deliver mRNAs (a type of nucleic acid) encoding immune-activating proteins to target immune cells. We will test whether nanoparticles loaded with the appropriate mRNAs can shrink or eliminate tumours in pre-clinical models of cancer, and will assess the global changes in the immune system induced by the various nanoparticle formulations.
This treatment has the potential to be utilized in multiple cancer types and could be combined with new blockbuster immunotherapies in the hope of defeating cancers in those patients in which previous therapy has failed.
The nanoparticle formulation screen itself is not limited to immune cells and can be easily adapted to screen for nanoparticles that best target any cell type within a complex population. We envision that the approach could be widely applied by other scientists who wish to identify optimal nanoparticle formulations for a given tissue or cell type.

PI: Kenneth Harder
Collaborators:
Pieter Cullis (UBC), Fabio Rossi (UBC), Ryan Vander Werff (BRC), Dominik Witzigmann (UBC)
Status:
Active – funding cycle: 2019-2021
Development and optimization of LNP-based gene therapy approaches in the brain
Theme II: Gene Therapy
Host institution: University of British Columbia
Brain diseases represent a significant burden to the Canadian health care system and it is estimated that the number of people affected by these diseases is increasing. The development of effective treatments for brain diseases, particularly age-related diseases such as Alzheimer’s and Parkinson’s disease, is a critical goal in terms of both economic and social impact for Canadians.
Gene therapy refers to different ways to correct defects in genes that cause human diseases. This is most commonly done by either removing something bad that is produced or by replacing something that is missing when a defective gene causes disease. Gene therapy in the brain is an attractive option for treating many different brain diseases (some examples of these types of brain diseases are Alzheimer’s disease, Parkinson’s disease, and Huntington’s disease), but we need to find better ways to deliver gene therapy to the brain.
A drug delivery method called lipid nanoparticles (LNPs) has been successfully used to deliver gene therapy products to the liver to treat liver disease. In this proposal, we will test how different types of LNPs can be used to deliver gene therapy to the brain. The identification of specific LNPs that effectively deliver gene therapy to the brain will provide the basis for future drugs to treat brain diseases. Packaging different kinds of gene therapy into LNPs suitable for use in the brain will advance the treatment of many kinds of human brain disease. This technology has the potential to benefit millions of Canadians and to help relieve the burden of these devastating brain diseases in our aging population.
See the presentation and poster by Sarah Thomson on this project: Development of lipid nanoparticle-enabled gene therapy approaches in the brain

Site-specific laser-mediated gene therapy for corneal endothelial diseases
Theme II: Gene Therapy
Host institution: Polytechnique Montreal
Ocular diseases affecting the cornea (the transparent front part of the eye) are leading causes of vision loss and affect millions of individuals worldwide. The progress of these ocular
diseases can be temporarily paused at certain stages using current therapies; however, the patients permanently suffer from incurable ocular disease.
Emerging solutions that interfere with defective genes or supplement deficient genes have shown promise. Nevertheless, there is a current void in treatment modalities that selectively target abnormal cells on the eye, which has hindered the development of effective gene therapies.
Several current gene delivery approaches call for the use of viruses to deliver genes, yet virus-based systems present a number of toxic side effects. A safe, precise and selective gene delivery system for abnormal cells would
open novel therapeutic avenues to address diseases that are of major public health concern.
This project aims to develop new therapeutic approaches for corneal diseases based on nanomaterials enhanced laser gene delivery and hence overcome the current pitfalls of classical delivery methods. This approach is based on the use of a laser and nanomaterials to generate transient pores (an adjustable range from a few nanometers to micrometers) in the membranes of target cells, enabling the delivery of desired transgenes.
The double specificity of conjugated nanomaterials targeting specific cell surface markers and fine-tuning of laser focalization over abnormal cell areas represents a clear advantage over current delivery systems. A provisional patent was recently filed on the new gene therapy protocol for ocular diseases. This project will address more specifically the feasibility of this new technique to treat blinding diseases (i.e., corneal endothelial dystrophies).

PI: Michel Meunier
Co-PIs:
Isabelle Brunette (Université de Montreal), Joseph Casey (University of Alberta), Przemyslaw (Mike) Sapieha (Université de Montreal)
Collaborators:
Pieter Cullis (UBC), Marianna Foldvari (University of Waterloo)
Partner:
Optima
Status:
Active – funding cycle: 2019-2021
Development and utilization of in vivo systems to optimize lipid nanoparticles for therapeutic genome editing: Focus on delivery to muscle for the treatment of LPL Deficiency
Theme II: Gene Therapy
Host institution: University of British Columbia
Less than 5% of human genetic diseases have approved gene therapy treatments and these treatments are often of low therapeutic benefit. This project will develop and optimize a novel therapeutic strategy that uses lipid nanoparticles (LNPS) to deliver CRISPR-based genome editing components to precisely repair disease-causing errors in a patient’s DNA. This will provide a scalable, cost-effective, and precise treatment that restores the endogenous expression and regulation of a target gene.
This strategy will also enable repeat dosing of the treatment to achieve optimal therapeutic benefit. Importantly, the universal components of this gene repair system could be applied to the treatment of thousands of different genetic diseases by simply re-targeting the CRISPR gene repair components to a different disease-specific site in the genome, for each different disease.
Initially, we will create two mouse models that we will use to optimize the delivery of genome editing
components by LNPs. Mice will be engineered to carry
“reporter” genes in their DNA with mutations that block the reporter “signal” of these genes. We will
then optimize the delivery of genome editing components to repair these specific mutations, thereby restoring the reporter gene signal, which will be readily detectable using whole animal imaging. We will initially focus on optimizing LNPs to deliver genome editing components into muscle, our initial target tissue for the treatment of LPL Deficiency.
The long-term goal of this research is to bring genome-targeted therapeutics into mainstream healthcare. Precision genome-editing could be broadly applicable to many genetic diseases, including cancer.

PI: Colin Ross
Co-Investigators:
Pieter Cullis (UBC), Sarah Hedtrich (UBC), Shy-Dar Li (UBC), Ramona Salvarinova (UBC), Dominik Witzigmann (UBC)
Collaborators:
David Liu (Harvard University), Anton McCaffrey (TriLink Biotechnologies Inc.), Elizabeth Simpson (UBC)
Partners:
Harvard University, MIT, TriLink Biotechnologies Inc.
Status:
Active – funding cycle: 2019-2021
SI: COVID-19 Therapeutics
Theme II: Gene Therapy
Host institution: University of British Columbia
This strategic initiative directly responds to the global need for COVID-19 therapies. It will produce a novel therapeutic treatment and potentially highly protective vaccine using lipid nanoparticle (LNP) and mRNA technology. The project will also inform clinical health response and decision making at national and international levels by providing comparative studies of potential therapeutics and vaccines.
A team at UBC will conduct research in mice aimed at identifying and selecting LNP-mRNA systems that provide an optimized SARS-CoV-2 neutralization and immune response to SARS-CoV-2. Promising lead candidates to cure (therapeutic) and prevent (vaccine) the viral infection will be identified and Acuitas Therapeutics will assess potency in non-human primates (NHP). If the NHP results are positive, we will identify a commercial partner and work with that partner to prepare an Investigational New Drug (IND) application to Health Canada to support a Phase I clinical trial.
More information | Read about the CIHR support for this initiative
PI: Pieter Cullis
Co-Investigators:
Jayesh Kulkarni (UBC), Dominik Witzigmann (UBC)
Collaborators:
Ninan Abraham (UBC), Janet Dancey (Canadian Cancer Clinical Trials Network), Manish Sadarangani (Vaccine Evaluation Center), Drew Weissman (University of Pennsylvania)
Partners:
Acuitas Therapeutics, Vaccine Evaluation Center
Status:
Completed – funding cycle: 2020-2021
SI: Pharmacokinetic profiling of gene expression after LNP-mRNA delivery to the brain using novel ionizable cationic lipids
Theme II: Gene Therapy
Host institution: University of British Columbia
This strategic initiative will identify the ionizable cationic lipid(s) that shows the highest efficacy and most favorable pharmacokinetic properties for delivery of nucleic acids to the brain. Once such a lipid is identified, we intend to create a strategy to broadly distribute the LNP formulation to academic collaborators and interested pharmaceutical companies for pre-clinical testing with individual therapeutic cargoes.
We have partnered with Acuitas Therapeutics to gain access to a wide range of proprietary ionizable cationic lipids that we will assess for efficacy of LNP delivery of nucleic acids in the brain.
The outcome of this proposal will be improved knowledge of how different ionizable lipids perform for delivery of nucleic acid drugs to the brain. We may identify a new brain drug delivery system with broad applicability to many different brain disorders.

Synthesis and Evaluation of Novel Sulfur-Containing Lipids
Theme II: Gene Therapy
Host institution: University of British Columbia
This research aims to produce novel fat-like substances (“lipids”) that enable the formulation of therapeutic RNA as minuscule globular bodies consisting of molecules of RNA associated with the foregoing lipids. At this time, this is the best way to administer RNA for treating human disease.
This project will unveil knowledge relating to the optimal structure of the lipids; relieve the burden of yet untreatable diseases; produce compounds with high market potential; and increase the standing and prestige of Canada as a world leader in the field of RNA therapeutics.

Developing a Long-Acting Prophylactic Treatment for Hemophilia using siRNA-Mediated Inhibition of Fibrinolysis
Theme II: Gene Therapy
Host institution: University of British Columbia
The overarching goal of this research is to develop a gene therapy that can enhance the lives of Canadians with bleeding disorders, particularly rare bleeding disorders that have limited treatment options.
This project will develop an siRNA-based gene therapy using lipid nanoparticles (LNPs) to precisely knock down the expression of proteins involved in degrading blood clots. The work will leverage our expertise in bioengineering and hemostasis biochemistry, and an international network of collaborators in gene therapy and clinical hematology.
We aim to develop this into a therapy that overcomes the limitations of current therapies to improve clinical care for Canadians with bleeding disorders, including rare bleeding disorders with limited treatment options, as well as hemophilia A and B. This technology can also be used as a scientific research tool, which could accelerate hemostasis and cardiovascular research.

Co-PIs:
Pieter Cullis (UBC), David Lillicrap (Queen’s)
Collaborator:
Timothy Nichols (UNC-Chapel Hill)
Status:
Active – funding cycle: 2020-2022
SI: NMIN Theme 2 Research & KTEE Accelerator
Theme II: Gene Therapy
Host institution: University of British Columbia
This KTEE strategic initiative will be implemented to maximize the translation and awareness of the knowledge/commercialization outputs of NMIN's Theme 2 (Gene Therapy) research projects.
A Research Accelerator/KT Specialist will be embedded within Theme 2 to work with the Research Leads, PIs, and NMIN Administrative Centre. This Research Accelerator/KT Specialist will: i) increase awareness, dissemination, and utilization of Theme 2 knowledge products (within NMIN and externally); ii) accelerate the commercialization potential of research results within Theme 2; and iii) enhance research management and knowledge mobilization expertise within NMIN Theme 2 and Network.

SI: Single-particle measurements to enable rational design of lipid nanoparticle carriers for gene therapies and vaccines
Theme II: Gene Therapy
Host institution: University of British Columbia
This research strategic initiative will apply CLiC imaging to measure the size and RNA loading of each individual nanoparticle in a sample population. This information is needed to develop new classes of therapeutics and discern complex sub-populations arising from biological complexity.
In partnership with ScopeSys Inc., a Canadian startup company commercializing CLiC technology for the development of biological therapeutics, the project aims to study RNA loading and release from lipid nanoparticle vehicles to characterize RNA delivery in vitro and in cells. These measurements are not possible with any other technique today, and are highly sought after by biotechnology and pharmaceutical companies involved in RNA-based drugs and vaccines.
This project will leverage the investigators' unique single-molecule and single-nanoparticle imaging expertise with the commercial avenues created by ScopeSys to bring a new assay to the pharmaceutical market. This assay will deliver the data needed to help guide the development of lipid nanoparticles for RNA-based therapeutics.
See the Research Presentation and poster by Albert Kamanzi based on this project: Single-particle microscopy of lipid nanoparticles and applications to vaccines and genetic medicines
PI: Sabrina Leslie
Collaborators:
Samuel Clarke (Precision Nanosystems Inc.), Pieter Cullis (UBC), Andreas Dahlin (Chalmers University of Technology), Joel Pedersen (University of Wisconsin at Madison)
Partner:
ScopeSys Inc.
Status:
Active – funding cycle: 2020-2021
Theme III: Diagnostics
Predicting nanoparticle tumour delivery via serum protein adsorption
Theme III: Diagnostics
Host institution: University of Toronto
When therapeutic nanoparticles are administered into the body, serum proteins stick to their surface. These proteins can influence how the nanoparticles are transported in the body and what cells and tissues they interact with. While many researchers consider this problematic (i.e., a fouling problem), this may be an opportunity.
There are two opportunities: (a) ability to use these serum proteins to determine how well the nanoparticles will accumulate at the cancer site; and (b) ability to use these serum proteins to diagnose the patient’s cancer or monitor treatment.
The significance of this development is that (a) profiling serum protein adsorption can be used for pre-screening of nano-formulations with the highest cancer delivery and therapeutic index; and (b) profiling serum protein adsorption may lead to
the development of simple blood-based diagnostics to effectively detect cancer patients or for monitoring therapeutic effectiveness of formulations.
To convert the utility of serum protein adsorption from a negative to a positive, there is a need to develop computational techniques to correlate the serum proteins with biological function.
The purpose of this project is to develop the predictive algorithms to correlate serum protein profiling with cancer delivery. This predictive algorithm will lead to collaborations with pharmaceutical, machine learning, and/or diagnostic companies, or could potentially lead to a new start-up company.
See the Research Presentation and poster by Johnny Zhang based on this project: An analysis of the function and structure of the protein corona on nanoparticles

PI: Warren Chan
Co-Investigator:Pieter Cullis (UBC)
Collaborator:Jonathon Krieger (Hospital for Sick Kids)
Status:Active – funding cycle: 2019-2021
Development of an integrated chip for exosome analysis in cancer
Theme III: Diagnostics
Host institution: University of Toronto
Sensitive and easy-to-use methods for the non-invasive detection of biomarkers could lead to new cancer screening tests for early diagnosis. Exosomes are released into the bloodstream by most cell types, including growing tumors. As exosomes are direct products of membrane-bound compartments of the cell, they can serve as circulating biomarkers for the tumour cells.
In this project, we aim to develop a novel microfluidic platform capable of isolating, sorting, and analyzing exosomes produced by cancer cells. We believe that this is a path that will lead to a powerful diagnostic device that could remotely detect changes in oncogenic profiles of inaccessible cancers in real time, through a simple blood test—a molecular liquid biopsy.
The technology is also amenable to the discovery of new markers for therapeutic development and companion diagnostics and will be broadly applicable to furthering the goals of other NMIN projects.
This technology will provide essential molecular information to clinical researchers and will provide molecular-level information from a patient blood sample to inform on disease progression.
See the Research Presentation and poster by Bill Duong based on this project: Development of a microfluidic chip for exosomal PD-L1 analysis in lung cancer

PI: Shana Kelley
Collaborators:
Stephane Angers (University of Toronto), Edward Sargent (University of Toronto)
Partners:
Cellular Analytics, NIH-NCE
Status:
Active – funding cycle: 2019-2021
On-Demand biofunctionalization of lipid nanoparticles for CAR T Cell Therapy
Theme III: Diagnostics
Host institution: University of Toronto
Nanomedicine is poised to deliver many paradigm-changing treatments; however, challenges remain to bring nanomedicine to broad patient populations and to remote or low-resource settings. We propose to address these challenges through the development of molecular tools for the low-cost, on-demand synthesis and conjugation of biologics for nanomedicine. Proof-of-concept work will demonstrate the manufacture of biologic therapeutics and their incorporation into lipid nanoparticles for CRISPR-based CAR T cell therapy to treat B-cell leukemia and lymphoma.
In the near-term, this project has exciting potential to accelerate nanomedicine research by making diverse and custom biologic therapeutics readily available to researchers, and to provide standardization to the drug conjugation process.
Our longer-term objective is to develop a technology that can improve patient access to nanomedicines through a series of advantages:
1) The therapeutic proteins (e.g. antibodies) that are attached to nanomedicine require constant refrigeration, which makes distribution of these drugs logistically challenging and costly. Our freeze-dried systems can be distributed at room temperature and, upon rehydration, can make these proteins on-site at the point-of-need.
2) Our approach decentralizes the manufacturing process and introduces the potential for inexpensive custom drug synthesis.
3)
This lower cost, coupled with the portable nature of our system, will ensure that nanomedicines can be delivered to patients more broadly, and in remote (e.g. northern communities), low-resource and global settings.
We have already validated the capacity of our molecular manufacturing technology with the production of over 50 therapeutics, including proteins (vaccines, conjugated antibodies) and small molecules. With this project, we aim to extend this capacity to nanomedicine with the development of the necessary technologies to enable the production and conjugation of antibodies to nanomedicine by any user. We will demonstrate this technology with the production of functionalized lipid nanoparticles (LNPs) for in vivo CD19-directed CAR T cell reprogramming and treatment of B-cell leukemia and lymphoma.
See the presentation and poster by Quinn Matthews on this project: A platform for automated functionalization of lipid nanoparticles for CAR T cell therapy

PI: Keith Pardee
Co-PI:Christine Allen (University of Toronto)
Collaborators:Pieter Cullis (UBC), Gilbert Walker (University of Toronto)
Status:Active – funding cycle: 2019-2021
A platform to screen for upregulation of soluble calreticulin as a tool to develop nanomedicines targeting acute myeloid leukemia
Theme III: Diagnostics
Host institution: University of Toronto
About 30% of acute myeloid leukemia (AML) patients suffer relapse in treatment which results in a poor
prognosis. Methods to detect and treat this patient population are needed. This project will develop new nanomedicines that have both diagnostic and therapeutic function.
It is hypothesized that the surface concentration of calreticulin (CRT) can be increased to enhance tumor cell recognition by tumor-associated macrophages and elicit therapeutic effects from the immune system. We aim to: 1) Identify drugs and drug combinations that enhance CRT expression; 2) Develop a microfluidic device able to determine CRT expression in AML patient derived cells; 3) Develop a drug combination product that would enhance CRT expression in treated AML patients and to correlate CRT expression with therapeutic responses.
The project will test the concept of a device to be used pre-clinically and clinically to assess CRT expression on AML cells. The device would serve to identify a drug combination that could be used to enhance CRT expression, in vitro and in vivo. We would work with NRC to identify unique anti-CRT targeted antibodies suitable for clinical development and conjugation to a nano-formulation of the selected product, and to explore scale-up device manufacture.
Better AML therapy will help people, including Canadians, to live longer, healthier lives. The market for AML therapy is expected to rise to more than USD $1.5B by 2026 in US, France, Germany, Italy, Spain, the UK, and Japan.

PI: Gilbert Walker
Co-PIs:
Mark Nitz (University of Toronto), Shan Zou (NRC)
Collaborator:
Chen Wang (Mt. Sinai Hospital)
Partner:
NRC
Status:
Active – funding cycle: 2019-2021
Customisable metallo-nanotexaphyrins for cancer imaging and therapy
Theme III: Diagnostics
Host institution: University of Toronto
The treatment of low volume oligometastatic cancers (e.g. prostate cancer) is currently limited by a lack of tools to precisely image and treat metastases. To address this unmet need, this project proposes a new class of nanoparticle theranostic agents, called nanotexaphyrins.
Nanotexaphyrins are composed of texaphyrin molecules that can bind many medically-important metal ions, such as lutetium (Lu) for cancer imaging and therapy. The idea is that the sheer number of texaphyrin molecules (>80,000) packed into a single nanoparticle, combined with the nanoparticle’s inherent ability to accumulation in tumor tissue, will lead to a significant enhancement in both the imaging sensitivity and therapeutic efficacy of metallo-nanotexaphyrin agents.
As a proof-of-concept, we propose to create a Lu-nanotexaphyrin with a mixture of “cold” and radioactive “hot” Lu. The “cold” Lu-nanotexaphyrin will permit potent photodynamic therapy whereas the incorporation of the “hot” Lu radioisotope will allow for non-invasive and sensitive radionuclide imaging (SPECT) and image-guided therapy. Specifically we will develop and optimize the mixed “hot” and “cold” Lu-
nanotexaphyrins to enable simultaneous non-invasive imaging, and image-guided focal photodynamic therapy with future applications for radionuclide therapy via higher “hot” Lu loading in this nanoparticle.
We will test our nanoparticles for SPECT imaging first in an orthotopic prostate tumour mouse model (Year 1). This will be followed by the evaluation of their image-guided therapeutic efficacy in both orthotopic prostate tumor mouse and (pilot) canine prostate tumour models (Year 2).
The successful completion of this proof-of-concept study will lay the foundation for a nanotexaphyrin agent with clinical theranostic utilities and lead to future licensing opportunities.

PI: Gang Zheng
Co-Investigators:
Marc Adler (Ryerson University), Raymond Reilly (University of Toronto)
Status:
Active – funding cycle: 2019-2021
SI: NMIN Theme 3: Research & KTEE Accelerator Project
Theme III: Diagnostics
Host institution: University of Toronto
This KTEE strategic initiative will be implemented to maximize the translation and awareness of the knowledge/commercialization outputs of NMIN's Theme 3 (Diagnostics) research projects.
A Research Accelerator/KT Specialist will be embedded within Theme 3 to work with the Research Leads, PIs, and NMIN Administrative Centre. This Research Accelerator/KT Specialist will: i) increase awareness, dissemination, and utilization of Theme 3 knowledge products (within NMIN and externally); ii) accelerate the commercialization potential of research results within Theme 3; and iii) enhance research management and knowledge mobilization expertise within NMIN Theme 3 and Network.

An ultrasensitive digital nanoassay for immunotherapy effectiveness
Theme III: Diagnostics
Host institution: University of Toronto
This project will develop a new type of “digital” nanoassay that is capable of being used to monitor ultralow abundant biomarkers that are associated with immunotherapy effectiveness.
The new test will be realized in an automated, sample-in/answer-out format relying on the digital microfluidics, a liquid handling platform in which arrays droplets can be manipulated over a "checkerboard"-like array of electrodes.
If successful, this strategy will serve as a valuable new technique to detect biomarkers related to the immunotherapies that are being developed at NMIN. In the long term, we plan to use the new technique to power companion diagnostics to identify patients who are most likely to respond to NMIN therapies.
See the presentation and poster by Sheldon Decombe on this project: An ultrasensitive digital nanoassay for immunotherapy effectiveness
Nanoparticle-enhanced, impedance-based biosensor development for cancer diagnostics
Theme III: Diagnostics
Host institution: University of Alberta
This project will develop a platform technology for point-of-care diagnostic testing for colon cancer based on detecting key small molecule biomarkers in urine using nanotechnology-based sensors.
The system will consist of a handheld electric reader and will use disposable electrode chips for processing urine samples. This system will use nanomaterials to improve sensitivity and enhance the signal, while automated microfluidics will be used to reduce testing time and make the system easy to use.
Once fully developed and tested, this technology will bring precision colon cancer diagnosis and screening to areas with limited access to healthcare or advanced diagnostic facilities. It will also allow point-of-care diagnosis and monitoring to take place in clinics or in patients’ homes.
See the Research Presentation and poster by Payton LeBlanc based on this project: Nanoparticle Enhanced, Impedance-Based Biosensor Development for Cancer Diagnosis
Core Facilities
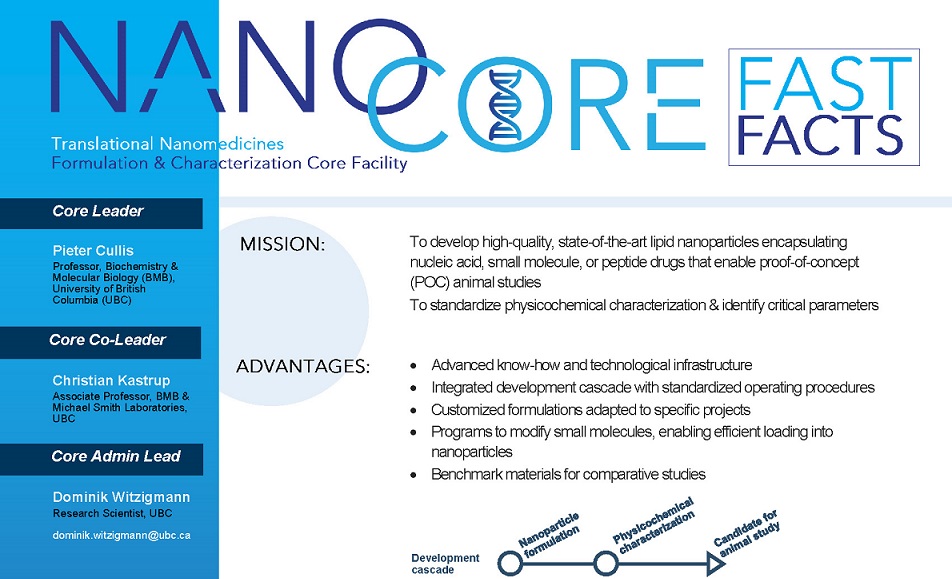
NanoCore:
Translational NanoMedicines Formulation & Characterization Core Facility
Core Facility
Host institution: University of British Columbia
Nanomedicines offer the possibility of drastically reducing suffering from genetic disorders, infections and cancer. Nanomedicine development requires a cohesive, collaborative effort that leverages resources from various disciplines.
The Translational NanoMedicines Formulation and Characterization Core Facility (NanoCore) facilitates NMIN's vision of translating nanomedicines to the clinic by providing state-of-the-art nanoparticle formulations and a standardized nanomedicines characterization service to enable potent therapies that can be readily manufactured.
The NanoCore serves as a NMIN resource and knowledge base to facilitate the development of new nanomedicines and will ensure that these new drugs have the potential to satisfy regulatory requirements.
Many NMIN investigators have considerable expertise in certain disease states but do not have extensive experience in formulating nanomedicine delivery systems.
NanoCore will provide these Investigators with the most advanced delivery technology possible, and also provide services such as nanoparticle reformulation, optimization, and lead selection.
By providing critical expertise and characterization services, NanoCore will accelerate the translation of nanomedicines into the clinic by ensuring that NMIN investigators are working with the most appropriate nanomedicine formulations required by their particular application.
Click on image to open a PDF of the NanoCore Fast Facts
Each slide is linked to the corresponding timepoint of the video.

PI: Pieter Cullis
Co-Investigators:
Christian Kastrup (UBC), Dominik Witzigmann (UBC)
Collaborators:Marianna Foldvari (University of Waterloo), Robert Hancock (UBC), Kenneth Harder (UBC), Christian Kastrup (Michael Smith Laboratories), Afsaneh Lavasanifar (University of Alberta), Blair Leavitt (UBC), Michel Meunier (Polytechnique Montreal), Colin Ross (UBC), Gilbert Walker (University of Toronto), Gang Zheng (University of Toronto)
Partners:
High Resolution Macromolecular, Integrated DNA Technologies
Status:
Active – funding cycle: 2019-2021
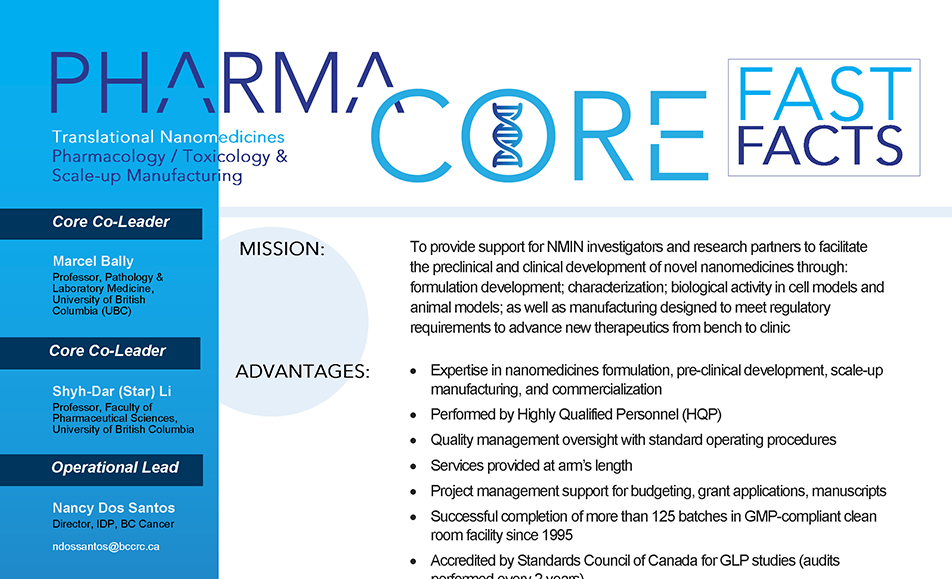
PharmaCore:
Preclinical, Scale-up Manufacturing & Project Management Core Facility
Core Facility
Host institution: University of British Columbia
To support NMIN’s mandate to translate nanomedicines from the bench to the clinic, PharmaCore provides support for NMIN Investigators to translate nanomedicines, which have been fully
characterized by the NanoCore, into clinical development candidates.
PharmaCore supports in vitro, in vivo studies as well as scale-up, stability testing and manufacturing needs to help exemplify
commercial potential. By bringing together Nanomedicine Investigators both in academia and industry, PharmaCore helps identify the best potential nanomedicines for commercial development, facilitates collaboration and helps with the formation of companies.
PharmaCore’s expertise will provide NMIN investigators and others in the network with the means to successfully develop novel nanomedicines into the clinical development stage leading to commercialization.
Click on image to open a PDF of the PharmaCore Fast Facts
Each slide is linked to the corresponding timepoint of the video.

PI: Marcel Bally
Co-PI:
Shyh-Dar Li (UBC)
Co-Investigator:Nancy Dos Santos (BC Cancer)
Status:Active – funding cycle: 2019-2021
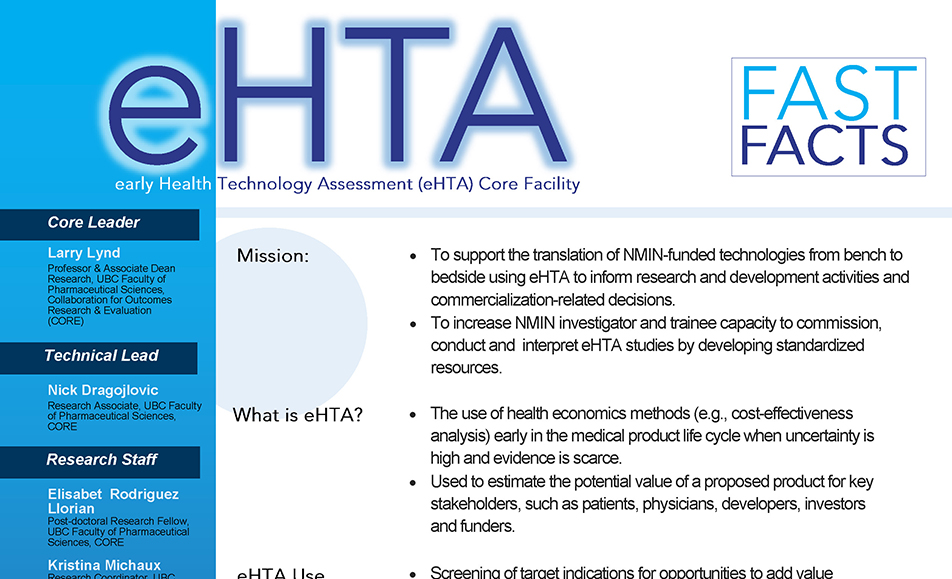
eHTA
An early Health Technology Assessment (eHTA) platform
Core Facility
Host institution: University of British Columbia
The primary role of the early Health Technology Assessment (eHTA) Core Facility is to help investigators craft a target product profile and position in the care pathway that maximizes the value for money their technology delivers to payers.
The Facility will apply and adapt standard economic evaluation and eHTA methods to answer the questions identified as most important for NMIN research teams. The core methodology will be cost-effectiveness/cost-utility analysis, which involves developing economic models to estimate the incremental cost and effectiveness of treating or testing patients with a technology relative to the next best alternative. The Facility will specialize in analyses that can be applied at early stages of product development when the comparative effectiveness and/or cost of implementation of the product is unknown.
The eHTA Core Facility will provide evidence-based tools and case studies in support of the commercialization of Network-supported intellectual property arising from NMIN-funded research projects. It also complements NMIN’s SI-Commercialization Support Program by facilitating the development of new and existing Canadian companies in the nanomedicines field with potential to generate social and economic benefits to Canadians.
Click on image to open a PDF of the eHTA Fast Facts
Each slide is linked to the corresponding timepoint of the video.

PI: Larry Lynd
Status:Active – funding cycle: 2021-2024