LRD 2022
PROGRAM
Agenda / Program
| Sunday, June 12 | Monday, June 13 | Tuesday, June 14 | Wednesday, June 15 | |
|---|---|---|---|---|
| 10:00 am |
Tea & coffee
- |
| Sunday, June 12 | Monday, June 13 | Tuesday, June 14 | Wednesday, June 15 | |
|---|---|---|---|---|
| 8:00 am |
Opening Remarks
- |
Opening Remarks
- |
Opening Remarks
- |
|
| 10:00 am |
Opening Remarks
- |
| Sunday, June 12 | Monday, June 13 | Tuesday, June 14 | Wednesday, June 15 | |
|---|---|---|---|---|
| 10:00 am |
LNP Systems & the Pharmaceutical Industry
- Tom Madden (Acuitas): Clinical Opportunities for messenger RNA-LNP Pharmaceuticals |
|||
| 10:30 am |
| Sunday, June 12 | Monday, June 13 | Tuesday, June 14 | Wednesday, June 15 | |
|---|---|---|---|---|
| 11:30 am |
Networking Lunch
- including mentoring/networking sessions with trainees & senior investigators in rooms 1410 & 1510 LSI |
|||
| 12:00 pm |
Networking Lunch
- including mentoring/networking sessions with trainees & senior investigators in rooms 1410 & 1510 LSI |
Networking Lunch
- including mentoring/networking sessions with trainees & senior investigators in rooms 1410 & 1510 LSI |
||
| 12:30 pm | ||||
| 1:00 pm |
| Sunday, June 12 | Monday, June 13 | Tuesday, June 14 | Wednesday, June 15 | |
|---|---|---|---|---|
| 9:30 am |
Networking break
- Poster Viewing |
|||
| 10:00 am |
Networking break
- Poster Viewing |
Networking break
- Poster Viewing |
||
| 10:30 am | ||||
| 2:00 pm |
Networking break
- Group Picture |
|||
| 2:30 pm |
Networking break
- Poster Viewing |
|||
| 3:00 pm |
Networking break
- |
|||
| 3:30 pm |
Networking break
- Poster Viewing |
|||
| 4:00 pm | ||||
| 4:30 pm |
Networking break
- Poster Viewing |
|||
| 5:00 pm | ||||
| 5:30 pm |
| Sunday, June 12 | Monday, June 13 | Tuesday, June 14 | Wednesday, June 15 | |
|---|---|---|---|---|
| 5:30 pm |
Opening Reception
- |
|||
| 6:00 pm | ||||
| 6:30 pm | ||||
| 7:00 pm | ||||
| 7:30 pm |
| Sunday, June 12 | Monday, June 13 | Tuesday, June 14 | Wednesday, June 15 | |
|---|---|---|---|---|
| 7:00 am |
Breakfast
- |
Breakfast
- |
Breakfast
- |
|
| 7:30 am | ||||
| 8:00 am |
| Sunday, June 12 | Monday, June 13 | Tuesday, June 14 | Wednesday, June 15 | |
|---|---|---|---|---|
| 8:00 am |
Keynote Speaker
- Lipids, Liposomes and Lipid Nanoparticles: Pieter Cullis (UBC | NMIN) |
|||
| 8:30 am |
Keynote Speaker
- Lipid nanoparticles for overcoming biological barriers to mRNA delivery Michael Mitchell (U Penn) |
Keynote Speaker
- Complexity & Reality: The Case of Thermosensitive Liposomes Christine Allen (U Toronto | NMIN) |
||
| 9:00 am |
|
|||
| 9:30 am | ||||
| 3:00 pm |
Keynote Speaker
- Nanomedicine Quo Vadis? Lessons Learned as Scientist, Developer & Entrepreneur Chezy Barenholz (Hebrew University of Jerusalem) |
|||
| 3:30 pm | ||||
| 4:00 pm |
|
|||
| 4:30 pm |
| Sunday, June 12 | Monday, June 13 | Tuesday, June 14 | Wednesday, June 15 | |
|---|---|---|---|---|
| 7:00 pm |
Banquet
- Robert H. Lee Alumni Centre, UBC |
|||
| 7:30 pm | ||||
| 8:00 pm | ||||
| 8:30 pm | ||||
| 9:00 pm | ||||
| 9:30 pm |
| Sunday, June 12 | Monday, June 13 | Tuesday, June 14 | Wednesday, June 15 | |
|---|---|---|---|---|
| 9:00 am |
Lightning Round Presentations
- Adjudicated Abstracts |
|||
| 9:30 am |
| Sunday, June 12 | Monday, June 13 | Tuesday, June 14 | Wednesday, June 15 | |
|---|---|---|---|---|
| 1:00 pm |
Invited Phospholipid Research Centre Lectures
- Introduction to the Phospholipid Research Centre (PRC) Bruce Baretz (PRC) Translational models to evaluate the performance of lipid based delivery systems Jörg Huwyler (U Basel) Targeted Liposomal Drug Delivery to Pediatric Sarcomas Michele Bernasconi (U Bern) Lipid self-assembling nanoparticle for RNA delivery: Toward personalized medicine Giuseppe De Rosa (U Naples Federico II) |
|||
| 1:30 pm | ||||
| 2:00 pm |
| Sunday, June 12 | Monday, June 13 | Tuesday, June 14 | Wednesday, June 15 | |
|---|---|---|---|---|
| 4:30 pm |
Poster Award Presentations
- In Memoriam (Andy Janoff) |
|||
| 5:00 pm |
| Sunday, June 12 | Monday, June 13 | Tuesday, June 14 | Wednesday, June 15 | |
|---|---|---|---|---|
| 5:00 pm |
LRD Business Meeting
- |
|||
| 5:30 pm |
| Sunday, June 12 | Monday, June 13 | Tuesday, June 14 | Wednesday, June 15 | |
|---|---|---|---|---|
| 6:30 pm |
Speakers' Dinner
- Cecil Green House |
|||
| 7:00 pm | ||||
| 7:30 pm | ||||
| 8:00 pm | ||||
| 8:30 pm | ||||
| 9:00 pm | ||||
| 9:30 pm |
| Sunday, June 12 | Monday, June 13 | Tuesday, June 14 | Wednesday, June 15 | |
|---|---|---|---|---|
| 3:00 pm |
Panel Discussion: Keynote Speakers
- LNP Technology-Past and Future |
|||
| 3:30 pm | ||||
| 4:00 pm | ||||
| 4:30 pm |
| Sunday, June 12 | Monday, June 13 | Tuesday, June 14 | Wednesday, June 15 | |
|---|---|---|---|---|
| 4:30 pm |
Closing Remarks
- |
This program may be subject to change and will be updated regularly.
Speakers

Christine Allen, Ph.D.
Dr. Christine Allen is the Associate Vice-President and Vice-Provost, Strategic Initiatives (AVPVP SI) at the University of Toronto. In this role, she leads the identification, assessment, prioritization and support of strategic, cross-divisional, excellence-driven, institutional initiatives. She is a full professor in the Leslie Dan Faculty of Pharmacy and holds a PhD in chemistry. Her research focuses on the design of innovative materials and drug delivery technologies. She is the co-founder and served as President of Nanovista Inc., a company focused on high-precision, image-guided cancer therapy. Professor Allen has received career awards from CIHR/Rx&D, the Canadian Society for Pharmaceutical Sciences (CSPS) and the Association of Faculties of Pharmacy of Canada. She is a fellow of CSPS, the American Institute for Medical and Biological Engineering, the Controlled Release Society (CRS) and the Canadian Academy of Health Sciences. She is the Editor-in-Chief of the Journal of Controlled Release and President-Elect of the CRS.

Theresa (Terry) Allen, PhD, FRSC, FCRS
Dr. Allen is Professor Emerita, retired a decade ago after a 40+ year career in drug discovery and drug delivery. Career highlights include research into the development of long-circulating liposomes (Doxil), ligand-targeted liposomes and ligand-targed LNPs. She continues to be active in consulting and strategic advising. Currently, she is a visiting professor at UBC, the chair of the Research Advisory Committee of the Nanomedicines Innovation Network (NMIN) and an organizer of LRD 2022.
Presentations: Opening remarks| 8:00 am Monday June 13 & LNP Technology—Past & Future Panel (Chair) | 3:20 Wednesday June 15

María J. Alonso, Ph.D.
María José Alonso is Professor of Pharmaceutical Technology at the University of Santiago de Compostela, Spain. Her lab has pioneered numerous discoveries in the field of nanomedicine. She has coordinated several research consortia financed by the WHO, the Gates Foundation and the European Commission.
She is the author of more than 300 scientific contributions with H factor 98. She is the inventor of 22 patent families, most of them licensed to industry and she has been part of 3 start-up ventures. Because of the quality of her scientific articles she has been among the TOP TEN in Pharmacology (Times Higher Education international ranking, 2010). Recently, she become part of the “Power List” of the most influential researchers in the field of Biopharmaceuticals (The Medicine Maker, 2020, 2021)
She has served to the Release Society (CRS) for 15 years and become President of the CRS in 2018. She is also Editor-in-Chief of the Drug Delivery and Translational Research, an official journal of the CRS, and she is part of the editorial board of 12 journals.
She has received 36 awards, among them the “Founders Award”, the “Outstanding Service Award” and the “Women in Sciences Award” of the CRS. She is a fellow of the AIMBE and a Fellow of the CRS, a member of the Royal Academy of Pharmacy of Spain, the Royal Academy of Sciences of Galicia, the Royal Academy of Pharmacy in Galicia a member of the Royal Academy of Medicine of Belgium and a member of the US National Academy of Medicine (NAM).
Carl Alving, MD
Dr. Alving received a B.S. from Haverford College; M.D. from University of Miami Miller School of Medicine; internship and residency in medicine and a fellowship in pharmacology at Barnes Hospital and Washington University in St. Louis. In 1970 he was drafted as a physician-scientist-soldier and served 30 years on active duty at the Walter Reed Army Institute of Research (WRAIR) and retired as a colonel. As a civil service employee, he was a medical officer, and supervisory scientist at WRAIR from 2000 to 2017, and is now Emeritus Senior Scientist. He is an adjunct professor of microbiology and immunology at the Uniformed Services University of the Health Sciences in Bethesda, MD.
He developed an early successful application of liposomes as drug carriers for treatment of leishmaniasis. He is the co-inventor of needle-free transcutaneous immunization by skin patch. He has been an author on 330 scientific publications in the fields of adjuvants, antigens, antibodies, complement, lipid biochemistry and immunology, and liposomes as drug carriers and carriers of vaccines. He has created adjuvants for experimental vaccines to malaria, HIV, meningococcal infection, heroin addiction, biological threat agents, prostate and intestinal cancer, Campylobacter diarrhea, and SARS-CoV-2. He holds 33 U.S. patents, the latest of which is Army Liposome Formulation with QS21 (ALFQ). His current research is focused on vaccines to HIV-1, malaria, and a universal influenza vaccine. He is a fellow of the American Association for the Advancement of Science; fellow of the National Academy of Inventors; and 3rd recipient of the Bangham Award.
Presentation: Army Liposome formulation with QS21 (ALFQ): A potent & safe vaccine adjuvant | 3:00 pm Monday June 13

Thomas L. Andresen, Ph.D.
Thomas L. Andresen is a Professor at the Technical University of Denmark (DTU) and CEO of T-Cypher Bio, an Oxford UK based gene and cell therapy company. He has previously been the founding Director of the Institute of the Health Technology at DTU and prior to that the Director of Institute of Nanotechnology. He was also the founding director of Center for Nanomedicine and Theranostics at DTU.
Prof. Andresen’s lab has been focused on research in biomaterials and nanotechnology towards development of new therapeutics and biomedical technology. His research has in particular focused on understanding biomaterial properties in the context of the interactions with biological barriers and interfaces. He has published more than 200 research articles and have been co-inventor of more than 50 pending and granted patents. He has co-founded 6 biotech and medtech companies, most recently Repertoire Immune Medicine in Boston as founding CSO, and T-Cypher Bio in Oxford as founding CEO. In addition, he is a board member and scientific advisory board member of several companies.
Marcel Bally, Ph.D.
Dr. Bally has focused his career on development of much needed novel drugs, drug combinations and drug delivery systems designed for use in patients with cancer. Dr. Bally received his BSc (1977) and MSc (1979) degrees in biology from Texas A&M University. He obtained his PhD from the Department of Biochemistry at the University of British Columbia (1984). He has recognized expertise in pharmacology/toxicology, drug formulations and preclinical cancer models. He is qualified to conduct preclinical safety studies under Good Laboratory Practices and has completed training in Good Manufacturing Practices. His scientific works (scientific articles, abstracts, book chapters and patents) have been cited >27,500 times. He has trained >65 highly qualified personnel; many of which now hold significant positions in industry, academia and medicine. He has co-founded multiple companies including Lipex (acquired by Northern Lipids), Inex (now Arbutus), Northern Lipids (renamed Transferra and purchased by Evonik in 2016), Celator (purchased by Jazz in 2016) and Cuprous Pharmaceuticals. Dr. Bally was one of the co-founders of Canada’s Centre for Drug Research and Development (joined with NEOMED to form adMare BioInnovations in 2019) as well as the Nanomedicine Innovation Network. The research he was part of contributed to the effort leading to three marketed drugs (Myocet- for metastatic breast cancer; Marqibo- for relapsed ALL and Vyxeos – for high risk AML).
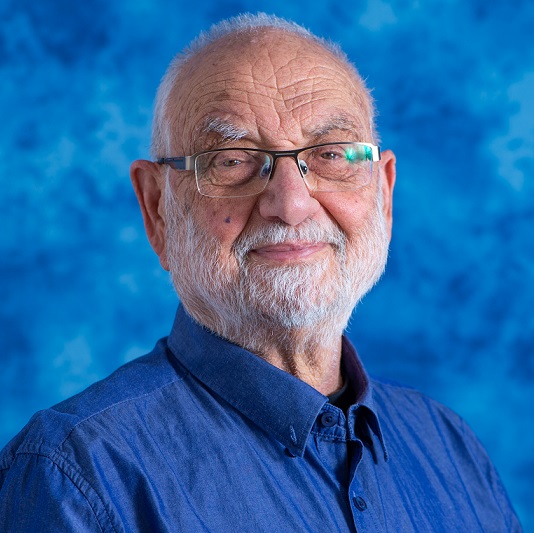
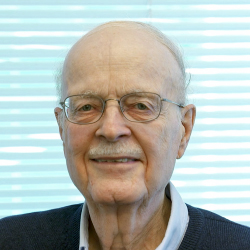
Yechezkel (Chezy) Barenholz , Ph.D.
Professor Emeritus Yechezkel Barenholz is at the Hebrew-University faculty since 1968, received Ph.D. in 1971, became a Professor in 1981. During 1973 to 2006 he was a visiting Professor and teaching, at the University of Virginia , He was also teaching at leading Universities world-wide (US, UK, Italy, Denmark, Japan, China, Australia).
Barenholz’s current research focuses on development of liposome-based nano-drugs, as best exemplified by the anticancer drug Doxil®, the first nano-drug approved by the FDA (November 1995) with over 700,000 cancer-patients treated so-far world-wide. Three of Barenholz’s other advanced liposomal nano-drugs developed by Barenholz and his team are: MMII liposomes for osteoarthritis treatment (now in phase II clinical trial); Nano-Mupirocin against resistant-bacteria is ready for clinical trials; and the local anesthetic Bupigel (LBL-100) is now in the scale-up stage).
Barenholz success stems from his major achievements in membrane biophysics including the concept of membrane “fluidity” and nanotechnology. Barenholz is author in >435 publications (cited >39,000 times, h-index 98). His research was supported by major grant agencies (NIH, EU, ISF, BSF, GIF Israel Ministry of Health, Israel Ministry of Science and others.). He is a co-inventor in >55 granted patents, half of them licensed, and founder of six start-ups: NasVax (now Therapix), Moebious, PolyPid, LipoCureRX, Ayana and ReBioticsRX (now ARMazore). He received many national and international awards related to Nano-Medicine, Nanotechnology and drug delivery including the 2012 CRS founder award and the 2020 Israeli Prime Minister EMET Prize for Exact Sciences (nanotechnology). On October 2021 FDA approved the Generic Doxil developed by Barenholz and his team now sold in the US.
Among Barenholz many contributions are: The “Barenholz Prize” to encourage excellence and innovation of Israeli Ph.D. students in Applied Sciences, being a founder and the head of the steering committee of the new BioMed-.MBA program at the Hebrew-University School of Business-administration, On 2021 this School, the Israel Medical Association and 8400 organization together with Barenholz initiated a program of Directors with expertise in BioMed aim to serve in boards of BioMed/biotech industries. All the latter aim at building the network needed for enabling a thriving Israeli BioMed ecosystem.
Professor Barenholz is married to Dr Hanna Barenholz together they have 4 daughters and 12 grandchildren.
Presentation: Nanomedicine Quo Vadis? | 3:05 pm Tuesday June 14

Bruce H. Baretz, Ph.D.
Dr. Bruce H. Baretz has a diverse background in several fields of science and to this day has many diverse interests. Prior to obtaining his Ph.D. (Chemistry) from Columbia University in the City of New York under his mentor Nicholas J. Turro, Ph.D., Dr. Baretz performed research on Inborn Errors of Metabolism at Yale University School of Medicine under the tutelage of Kay Tanaka, M.D. The research focused on minor pathways of amino acid metabolism using stable isotopes and GC/MS, as well as synthesis of short chain isotopically labeled acids and diagnostic clinical testing of newborns. His research in Chemistry focused on many areas including magnetic field effects on radical pair chemistry, time resolved CIDNP studies, polymer: surfactant complexes, and cyclodextrin inclusion complexes, zeolite adsorbates and micellar supramolecular aggregates using fluorescence probes and modification of chemical reactions within.
Dr. Baretz has been in industry for over 40 years, initially with American Cyanamid Company, then with DNA Biochip programs with Siemens Medical and white light-emitting LEDs programs with Cree, Inc. For the last 16 years, Dr. Baretz has been with Lipoid LLC promoting the use of safe natural and synthetic phospholipid supramolecular assemblies for Drug Delivery, including liposomes, SLNP’s, micelles, pulmonary solid-state particles/dispersions, topical and ophthalmic implementations, as well as various vaccine programs, the last decade as President of Lipoid LLC. Lipoid LLC sells within North America the phospholipids manufactured by the cGMP facilities of Lipoid GmbH and Phospholipid GmbH in Germany, all inspired by Dr. Herbert Rebmann, our founder and leader for many years.
In addition to his focus on safe use of phospholipids in therapeutics and vaccines, Dr. Baretz retains an academic interest in trying to understand thermodynamics, especially that associated with self-assembly, as well as the thermodynamics of thermal radiation, and wondering where the end of an electro-magnetic wave goes, and at what rate, when the wavefront is incident on matter which absorbs the radiation. He has 16 publications and 16 patents associated with his research.

Michele Bernasconi, Ph.D.
Michele Bernasconi obtained his PhD in cell biology from the ETH Zurich. After a postdoctoral stay at the National Children Hospital in Tokyo, with a fellowship from the Japanese Science and Technology Agency, in 2000 he joined the lab of Prof. Ruoslahti at the Burnham Research Institute in La Jolla, CA, to work on in vivo phage display, with a postdoc fellowship of the Swiss National Science Foundation. From 2002 to 2018 he was group leader at the University Children’s Hospital in Zurich focusing on tumor targeting strategies for pediatric sarcomas. In 2015 he obtained a habilitation in Experimental Pediatric Oncology from the University of Zurich. Since 2018 he is head of the laboratory research at the Department of pediatric Hematology and Oncology of the Insel University Hospital in Bern. He is author of 40 peer-reviewed original research articles and one book chapter.
Anna Blakney, Ph.D.
Anna Blakney is an Assistant Professor in the Michael Smith Laboratories and School of Biomedical Engineering at UBC. She received her Bachelor of Science in Chemical & Biological Engineering from the University of Colorado at Boulder, and her PhD in Bioengineering from the University of Washington. She completed a postdoctoral fellowship at Imperial College London on the development of molecular and biomaterial engineering strategies for delivery of self-amplifying RNA. Her lab uses bioengineering, molecular biology and immunology approaches to develop the next generation of RNA vaccines and therapies.
Presentation: Optimization of Lipid Nanoparticles for Self-Amplifying RNA Expression and Cellular Activation Using a Design-of-Experiment Approach | 3:30 pm Monday June 13

Stephen Burgess, Ph.D.
Dr. Stephen Burgess serves as Managing Director of Avanti Polar Lipids, and he is Head of Lipid Technology & Nucleic Acid Delivery for Croda Pharma, supporting the Group’s vision to become the global leader in empowering biologics delivery. He has been associated with Avanti for over 40 years, starting as a part-time laboratory technician during high school and college. After receiving his doctorate in Biochemistry and Biophysics from The University of North Carolina – Chapel Hill in 1990, Dr. Burgess returned to Avanti as Director of Research & Development. Over the past 30 years, he has worked with numerous researchers to develop novel lipids and lipid formulations to address specific experimental challenges and improve drug delivery. He has played a key role in a diverse list of projects, including drug delivery development, gene therapy, wound healing, and vaccine development. His background in lipid synthesis, lipid biophysical properties, and membrane dynamics has been instrumental in resolving problems associated with these projects. Dr. Burgess is an author of numerous scientific publications, as well as an inventor on multiple patents.
Pieter R. Cullis, Ph.D., FRSC, FNAI (USA), OC
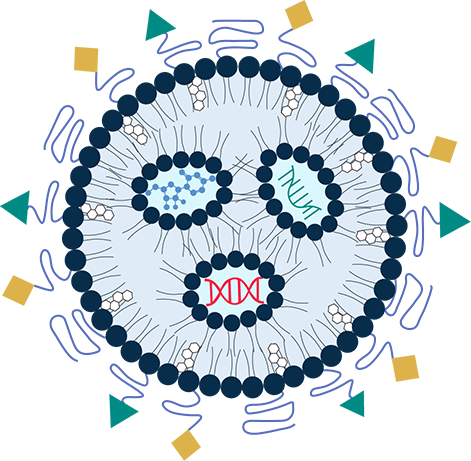
Pieter R. Cullis is Director of the Nanomedicines Research Group and Professor of Biochemistry and Molecular Biology at the University of British Columbia. Dr. Cullis and co-workers have been responsible for fundamental advances in the development of nanomedicines employing lipid nanoparticle (LNP) technology for cancer therapies, gene therapies and vaccines. This work has contributed to five drugs that have received clinical approval.
Dr. Cullis has co-founded eleven biotechnology companies that now employ over 300 people, has published over 350 scientific articles (h index 128) and is an inventor on over 60 patents. He has also co-founded two National Centre of Excellence networks, the Centre for Drug Research and Development (now AdMare) in 2004 and the NanoMedicines Innovation Network in 2019. These not-for-profit networks are aimed at translating basic research into commercially viable products.
Dr. Cullis has received numerous awards including the Order of Canada in 2021 and the VinFuture Prize (Vietnam), the Prince Mahidol Award (Thailand) and the Gairdner International Award (Canada) in 2022.
Two recently approved drugs that are enabled by LNP delivery systems devised by Dr. Cullis, members of his UBC laboratory and colleagues in the companies he has co-founded deserve special emphasis. The first is Onpattro which was approved by the US FDA in August 2018 to treat the previously fatal hereditary condition transthyretin-induced amyloidosis (hATTR). Onpattro is the first RNAi drug to receive regulatory approval. The second is Comirnaty, the COVID-19 vaccine developed by Pfizer/BioNTech that has received regulatory approval in many jurisdictions including Canada, the USA, the UK and Europe. Comirnaty is playing a major role in containing the global Covid-19 pandemic with approximately 3B doses administered worldwide in 2021.

James Dahlman, Ph.D.
James Dahlman is the McCamish Early Career Professor in the Department of Biomedical Engineering at Georgia Tech and Emory School of Medicine. His lab works at the interface of chemical engineering, genomics, and gene editing by applying big data approaches to nanomedicine. His trainees have developed DNA barcoded nanoparticles to measure how hundreds of nanoparticles deliver mRNA and siRNA in multiple cell types from a single animal in vivo, and the lab uses these approaches to deliver RNA outside the liver without targeting ligands. James was a co-founder and Board Chairman of Guide Therapeutics, which was acquired by Beam Therapeutics.

Giuseppe De Rosa, Ph.D.
Giuseppe De Rosa is full professor at the Department of Pharmacy, University of Naples Federico II.
He obtained a PhD in Pharmaceutical Technology in 2001 at the University of Cagliari, then he worked as post-doc fellow at the University Paris-Sud/UMR CNRS 8616 (France). In 2002 he became Assistant professor and in 2014 associate professor in Pharmaceutical Technology at the University of Naples Federico II.
His scientific activity is focused on design and development of drug delivery systems based on micro- and nanotechnologies, especially liposomes and self-assembling nanoparticles for systemic or topical administration. He is author of about 100 papers (H-index: 34) on peer review journals, different book chapters and patent applications/granted. Member of the editorial board of different journal in the field of Pharmaceutics. For his research activity, Dr De Rosa received different financial support, among them one by MIUR (Italian Minister for the University and Research), Ministero della Salute (Italian Minister of Health) and the Phospholipid Research Center of Heidelberg (Germany). He is member of the ADRITELF Board, and was member of the Board of the Controlled Release Society (CRS) Italy Chapter.

Philip Felgner, Ph.D.
Dr. Felgner made a series of discoveries that launched active fields of non-viral gene delivery systems and nucleic acid vaccines. The science is rooted in the topic of his post-doctoral research in Tom Thompsons laboratory and his mentor Chezy Barenholz – the biophysics, structure, and hydrodynamic properties of bilayer membranes. In 1980 there were no positively charged bilayer forming lipids available in nature to prepare stable positively charged lipid vesicles. In 1984 he collaborated with chemists at Syntex Research Institute to synthesize and characterize a series of positively charged bilayer forming lipids. When these vesicles interact with negatively charged nucleic acid the lipids and the nucleic acid reorganize together into a new lipid nanoparticle called ‘Lipoplex’ capturing 100% of the input nucleic acid. Lipoplexes are synthetic virus-like particles that deliver functional nucleic acid into cultured cells and ‘Lipofection’ has since become a leading in vitro transfection method used in laboratories worldwide. Then Felgner published highly cited reports showing functional gene transfer of plasmid DNA and mRNA into mouse muscle in vivo. This work spawned new fields of synthetic non-viral gene delivery systems and nucleic acid vaccine science.
More recently Felgner developed a protein microarray platform to measure antibodies levels induced after infection and vaccination against thousands of individual antigens derived from dozens of infectious microorganisms. At the beginning of the COVID outbreak his Coronavirus Antigen Microarray (COVAM) was poised to measure SARS-CoV-2 mRNA vaccine induced Ab levels against dozens of respiratory virus antigens and to measure the phenomenal success of the mRNA vaccines so important to the world today.
Presentation: 100 Years of Vaccine Science | 4:15 pm Tuesday June 14

Anne Frederica Grobler, Ph.D.
Prof. Anne Grobler has a PhD in Pharmaceutics (North-West University) and an MSc in Medical Biochemistry (Stellenbosch University). Her interest is the design and construction of nano-medicines and bio-agricultural delivery systems. She has worked at the University of Stellenbosch and North-West University, the SAMRC, and in the private sector (head of R&D at MeyerZall Laboratories, and at Austell Pharmaceuticals and now heads the Pheroid Cluster Incubator. She is a co-author of the SA Synthetic Biology Strategy, the SA Bio-Design Initiative and the Ministerial Review of STI institutions (2017). She established the Safety Pharmacology Society Group for SA and has founded spin-off companies including The Pheroid Cluster Incubator NPC, BioPher Pty Ltd, Antech Pharmaceuticals (Pty) Ltd and Inopher (Pty) Ltd She authored/co-authored 139 ISI publications and is an inventor/author of 9 patents granted or under examination. Her awards include: NIPMO Innovators Award for most disclosures with commercial potential at the NWU (2019), BioFundi Award for Research by the Gauteng Province and Innovation Hub (2018), the NWU Innovation Evangelist Award (2017), the NSTF/BHP Billiton Award for her contribution to SETI (2014); the Swiss Bio-technology Innovation Award, Switzerland (2011); two Vice Chancellor’s Honorary Award countries (2010).

Hideyoshi Harashima, Ph.D.
Hideyoshi Harashima is a Professor of Pharmaceutics and the chair of Laboratory for Molecular Design of Pharmaceutics, Faculty of Pharmaceutical Sciences, Hokkaido University. He received B.S., M. S. and Ph. D. from The University of Tokyo. After a post-doctoral training in School of Medicine at Stanford University, he became an Associate Professor at Faculty of Pharmaceutical Sciences, The University of Tokushima in 1989. He was appointed a Full Professor of Laboratory for Molecular Design of Pharmaceutics at Hokkaido University in 1999. He was also appointed a Professor of a newly build Laboratory of Innovative Nanomedicine in 2009. He became a Distinguished Professor of Hokkaido University since April, 2022.
He served as an Associate Editor of the Journal of Controlled Release (2009 – 2020) and Cancer Science (2009 – now) and as an Executive Editor of Advanced Drug Delivery Reviews (2012 – 2020). He was a president of Academy of Pharmaceutical Science and Technology of Japan (APSTJ: 2012 – 2014). He received The Nagai Award from Japanese Society of Drug Delivery System in 2007, Distinguished Science Award from FIP in 2010, Fellow from Controlled Release Society in 2013, APSTJ award and 19th SONG EUM Med-Pharm Award from Song Eum Academy Foundation in 2016. He also received Høst Madsen Medal from FIP in 2021. He published 435 original research articles, 70 invited reviews, 13 Book Chapters and 85 patent submissions.

Sarah Hedtrich, Ph.D.
Dr. Hedtrich obtained her PhD in Pharmacology & Toxicology from the Freie Universität Berlin in Germany in 2009. During her postdoc, she moved to the Ludwig-Maximilians-University in Munich and Tufts University in Boston, USA. After returning to Berlin 2013, she headed a junior research group and was appointed an assistant professor in 2015. She relocated her lab to the U of British Columbia in 2019. She co-/authored over 80 peer-reviewed journal articles in high impact journals including the Journal of Controlled Release, Small, Nature Reviews Materials, and Theranostics. Her research focuses on inflammatory and genetic diseases of human epithelia, the development of novel therapeutic approaches and tissue engineering of complex, human-based organ models aiming for valid and predictive test systems for preclinical and fundamental research.

Leaf Huang, Ph.D.
Leaf Huang is the Fred Eshelman Distinguished Professor, in the Eshelman School of Pharmacy, University of North Carolina at Chapel Hill. Dr. Huang’s research has been in the area of gene therapy and targeted drug delivery. He has pioneered the liposome non-viral vector and has designed and manufactured the cationic lipid vector for the first non-viral clinical trial in 1992. He was also the first to publish the activity of polyethylene glycol (PEG) in prolonging the circulation time of liposomes. His current work centers on nanoparticle vectors for gene transfer in tumor and liver. He also continues research in establishing a ligand targeted delivery system for cDNA, mRNA, siRNA, proteins and peptides for tumor growth inhibition and for vaccines in treating cancer and infected diseases. He has authored or co-authored more than 600 papers with an H-index of 137. He is also the inventor or co-inventor of 22 US and foreign patents. In 2004, he received the Alec D. Bangham MD FRS Achievement Award, which is the highest honor in liposome research. He was the recipient of the 2013 Distinguished Pharmaceutical Scientist Award which is the highest scientific recognition of the American Association of Pharmaceutical Scientists. He was named a Highly Cited Researcher in “Pharmacology & Toxicology” and then in “Cross Field” each year since 2016. Dr. Huang has also co-founded 6 biotech start-ups in the past.
Presentation: Liposomal Antibiotics Induce Anticancer Immunity by Killing the Tumor-Associated Bacteria | 1:40 pm Wednesday June 15

Jörg Huwyler, Ph.D.
Prof. Dr. Jörg Huwyler is full professor and head of the Division of Pharmaceutical Technology, Department of Pharmaceutical Sciences, University of Basel. His research interests are in the field of drug delivery and drug targeting using particulate drug carriers. Important professional milestones after his PhD in biochemistry and a habilitation in pharmacy were appointments at the University Hospital of Basel and the Brain Research Institute, UCLA School of Medicine, Los Angeles. From 1999 to 2006 he joined the pharmaceutical industry, where he worked as DMPK project leader for F. Hoffmann-La Roche Ltd. in Switzerland.

Lloyd Jeffs, Ph.D.
Dr. Lloyd Jeffs joined Precision NanoSystems (PNI) in June 2018. His Biopharma Services team is responsible for developing and executing custom programs to meet the clinical manufacturing needs of PNI’s clients. Lloyd is an expert in developing lipid-based nanotherapeutics and has over 20 years of experience in this field, including formulation and process development, scale-up and technology transfer.
Dr. Jeffs received his PhD. in Applied Microbiology from the University of Saskatchewan and has B.Sc. and M.Sc. degrees from the University of British Columbia. He is a co-author of numerous peer-reviewed publications dealing with the development of lipid nanoparticle therapeutics and is a co-inventor for key patents in this field.

Gerard M. Jensen, Ph.D.
Vice President of Operations, Gilead Sciences Inc.
Gerard M. Jensen earned a B.S. in Biochemistry from U.C.L.A. and a Ph.D. in Physical Chemistry from the University of Southern California, and then completed a post-doctoral fellowship in Molecular Biology at The Scripps Research Institute. His academic research has involved chiroptical and electron paramagnetic resonance spectroscopies, theoretical modeling of metalloproteins, site-directed mutagenesis, protein X-ray crystallography, and experimental and theoretical study of protein cavities.
At NeXstar Pharmaceuticals and later Gilead Sciences, he has led efforts in formulation development, scale-up and manufacturing of liposomal and oligonucleotide based therapeutics. He is presently the Vice President of Operations at the Gilead commercial manufacturing facility in San Dimas California and a new facility in La Verne California which provide manufacturing and support for Gilead sterile products worldwide. Products developed, approved, manufactured and commercialized from this site include AmBisome® (liposomal amphotericin B injection), a product that treats life threatening fungal infections, DaunoXome® (liposomal daunorubicin citrate for injection), a product that treats Kaposi’s sarcoma, Macugen® (pegaptanib sodium injection) an oligonucleotide aptamer treatment for age-related macular degeneration, and Veklury® (Remdesivir) for the treatment of COVID-19.
Dr. Jensen has been an Adjunct Professor at the Keck Graduate Institute in Claremont, at the California State University at Fullerton, the California Polytechnic State University at Pomona, and Azusa Pacific University. Dr. Jensen is an Associate Editor of the Journal of Liposome Research and has authored or co-authored over 40 publications or patent applications.

Christian Kastrup, Ph.D.
Dr. Christian Kastrup is a Senior Investigator at the Versiti Blood Research Institute and a Professor at the Medical College of Wisconsin in the Department of Surgery, with secondary appointments in the Departments of Biochemistry, Biomedical Engineering, and Pharmacology and Toxicology. He recently moved his laboratory from the University of British Columbia, where he is currently an Affiliate Professor. Christian is a biochemist who uses biotechnology to understand and control blood clotting proteins. He is passionate about controlling blood clotting because hemorrhage is a leader killer of young people, and thrombosis causes heart attacks, strokes and deep vein thromboses. His lab creates drug delivery systems and RNA and protein therapeutics toward addressing these issues. They work with the Canadian Armed Forces and the US Army. Christian has trained and supervised over a hundred researchers in his laboratory with these shared goals.

Jayesh A. Kulkarni , Ph.D.
Dr. Kulkarni obtained his PhD from the University of British Columbia and has over 10 years of academic and industry experience in the nanoparticle drug delivery field. He has published over 35 peer-reviewed articles in prestigious journals. He has held many awards, including the inaugural Nanomedicines Innovation Network’s postdoctoral fellowship in gene therapy. Dr. Kulkarni’s research has focused on the role of the various lipid components in LNP and the biophysics that governs particle formation. His work has contributed to clinical translation, including scale-up and manufacturing of LNP systems in accordance with GLP and GMP regulations. Dr. Kulkarni is a leader in the design and development of lipid nanoparticle (LNP) formulations of small molecule and nucleic acid therapeutics. He currently serves as the Chief Scientific Officer of NanoVation Therapeutics, an LNP-RNA formulation developer
Shyh-Dar (Star) Li, Ph.D.
Dr. Li is a Professor at UBC Faculty of Pharmaceutical Sciences. His research focuses on developing novel nanoparticles for targeting drugs to specific sites to enable novel therapeutics. His research program has been supported by federal funding, including CIHR and NSERC.

Thomas D. Madden, Ph.D.
President & CEO of Acuitas Therapeutics, Dr. Thomas D. Madden is a world-renowned expert in the area of nanotechnology. He co-founded Acuitas in February 2009 and has led the company into a position of global leadership.
Dr. Madden obtained his BSc. and Ph.D. in Biochemistry from the University of London, U.K. He has held several senior academic and industry positions including Assistant Professor in Pharmacology at the University of British Columbia and Senior Director, Technology Development and Licensing at Tekmira Pharmaceuticals.
At Tekmira, Dr. Madden was responsible for the development of several liposomal anticancer agents including Marqibo™ (liposomal vincristine), Alocrest™ (liposomal vinorelbine) and Brakiva™ (liposomal vinorelbine). All of these were subsequently licensed to Talon Therapeutics. He headed the team that developed the cationic lipid MC3 and the LNP carrier used by Alnylam Pharmaceuticals for Onpattro™. Recently, Dr. Madden led the development of the LNP carriers used in COMIRNATY®, a highly effective and safe COVID-19 mRNA vaccine produced through a partnership with BioNTech and Pfizer.
Dr. Madden has earned a reputation for collaboration. He credits the success of Acuitas Therapeutics and its exceptional standing on the world stage to the team’s commitment to excellence.
Dr. Madden has over 60 publications in peer-reviewed journals relating to LNP technology and the development of pharmaceutical products, including recent publications in Nature. In 2020, Dr. Madden was made a Fellow of the American Institute for Medical and Biological Engineering (AIMBE) in recognition of his contributions to the field of nucleic acid delivery.
Presentation: Clinical Opportunities for messenger RNA-LNP Pharmaceuticals | 10:20 am Sunday June 12

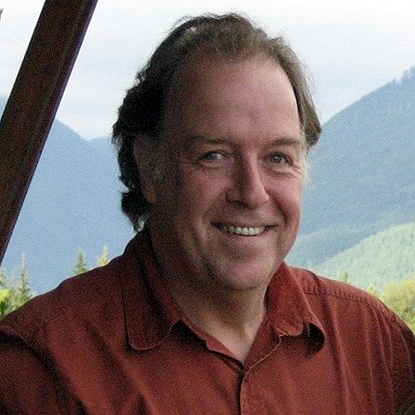
Michael Mitchell, Ph.D.
Michael J. Mitchell is the Skirkanich Assistant Professor of Innovation in the Department of Bioengineering at the University of Pennsylvania.
He received a BE in Biomedical Engineering from Stevens Institute of Technology in 2009, a PhD in Biomedical Engineering with Prof. Michael King from Cornell University in 2014. He was a Postdoctoral Fellow in Chemical Engineering with Prof. Robert Langer at MIT from 2014-2017, prior to pursuing his independent career at University of Pennsylvania. The Mitchell lab’s research broadly lies at the interface of biomaterials science, drug delivery, and cellular and molecular bioengineering to fundamentally understand and therapeutically target biological barriers. Specifically, his lab engineers new lipid and polymeric nanoparticle platforms for the delivery of different nucleic acid modalities to target cells and tissues across the body. His lab applies their research findings and the technologies developed to a range of human health applications, including the engineering of CAR T cells for cancer immunotherapy, mRNA vaccines, genome editing, cardiovascular disease, and in utero therapeutics to treat disease before birth.
Dr. Mitchell has received numerous awards as an independent investigator, including the National Institutes of Health Director’s New Innovator Award, the Rising Star Award from the Biomedical Engineering Society, and the Career Award at the Scientific Interface from the Burroughs Wellcome Fund. In 2022 Mitchell was named “Emerging Inventor for the Year” by Penn’s for Innovation in recognition for his lipid nanoparticle technologies and received the Young Investigator Award from the Society for Biomaterials, the T. Nagai Award from the Controlled Release Society, and the National Science Foundation CAREER Award.
Presentation: Lipid nanoparticles for overcoming biological barriers to mRNA delivery | 8:30 am Wednesday June 15

Roger Pak, Ph.D.
Roger is an Associate Research Fellow in BioTherapeutics Pharmaceutical R&D at Pfizer, Andover, MA and is focused on novel drug delivery technologies. He has more than 20 years industrial experience working at Bristol-Myers Squibb, Infinity Pharmaceuticals, Wyeth and Pfizer. During this time, he had worked on a number of drug products in clinical and commercial stage and a wide variety of drug delivery technologies such as antibody-drug conjugates, polymer conjugates and targeted nanoparticles. Roger received his Ph.D. in Chemistry from the University of California-Los Angeles (UCLA) and was an NIH Postdoctoral Fellow at the University of California-Davis. He also held fellowships at Argonne National Laboratories, University of Notre Dame and the City of Hope National Cancer Institute.
At Pfizer, he leads the efforts on lipids, polymers and conjugation technologies related to nanoparticles and biotherapeutic drug delivery that are applied within Pfizer’s pipeline portfolio. Recently, he led the team that was focused on developing the novel lipid excipients used in Pfizer/BioNTech’s Covid-19 vaccine (Comirnaty®).
Presentation: Novel Lipid Excipient Development for the Covid-19 mRNA Lipid Nanoparticle Vaccine | 2:20 pm Monday June 13

Norbert Pardi, Ph.D.
Dr Norbert Pardi holds a Ph.D. in biochemistry and genetics. He has been working at the University of Pennsylvania since 2011 and currently holds an Assistant Professor position at the Department of Microbiology of the Perelman School of Medicine. His research interest is the development of mRNA-based therapeutics with particular focus on new generation infectious disease vaccines. He explored the development of a novel vaccine platform using nucleoside-modified mRNA in lipid nanoparticles (LNPs) and used it to generate highly effective vaccines targeting various pathogens (influenza virus, coronaviruses, malaria and others). Dr. Pardi is a pioneer of the nucleoside-modified mRNA vaccine technology and published milestone papers in the field.

Presentation: The role of mRNA delivery system and route of administration on vaccine potency | 11:40 am Wednesday June 15

Syed Reza, Ph.D., MD
Syed Reza serves as a drug delivery consultant to NOF Corporation since 2017. In this role, Syed has been responsible for managing industry partnerships for NOF’s COATSOME technology and advises on strategic partnerships and licensing. Previously, Syed was Head of US Business Development for Octoplus N.V. and managed industry alliances and partnerships for Octoplus’ protein nanoparticle technology platform. Prior to that, Syed served as Director of Business Development for Hoffman LaRoche’s peptide technologies group in Colorado. He is a graduate of the New Jersey Medical School with an MD and Ph.D. in Molecular Biology.

Colin Ross, Ph.D.
Colin Ross, BSc(h) (UBC), MSc (Newcastle, UK), PhD (McMaster University), is Associate Professor, Faculty of Pharmaceutical Sciences, UBC, and a Scientist at B.C. Children’s Hospital Research Institute.
My research seeks to integrate genetics with novel strategies to improve the safety and effectiveness of medications. For example, I developed a novel gene therapy treatment for LPL Deficiency, a genetic disorder of lipid metabolism, which recently became one of the first gene-based therapies to receive regulatory approval. My research in this area is focused on viral and non-viral approaches for gene augmentation and therapeutic genome editing.

Gaurav Sahay, Ph.D.
Gaurav Sahay is an Associate Professor in the Department of Pharmaceutical Sciences, College of Pharmacy at Oregon State University. Dr. Sahay’s lab is developing novel nanotechnology-based platforms including lipid-based nanoparticles for effective delivery of messenger RNA therapeutics for treatment of cystic fibrosis, retinal degeneration and against SARS-CoV2. He has done pioneering work to dissect the intracellular transport essential for nucleic acid delivery to the cytosol and developed methods to overcome endosomal barriers. Dr. Sahay has more than 50-peer-reviewed publications in top tier journals including Science Advances, Nature, Nature Communications, Nature Biotechnology, Nature Nanotechnology, Journal of Controlled Release, Nano Letters etc. He is the winner of a 2013 American Association of Pharmaceutical Scientists (AAPS) Postdoctoral Fellow Award, the 2015 Controlled Release Society (CRS) T. Nagai Award, a 2016 American Association of Colleges of Pharmacy (AACP) New Investigator Award, a 2019 Oregon Health & Sciences University (OHSU) Distinguished Faculty Senate Award for Collaboration, 2020 Phi Kappa Phi OSU Emerging Scholar Award and 2020 CMBE Young Innovator Award. Sahay lab is funded through the NHLBI, NEI, Cystic Fibrosis Foundation, and several biotech companies. He serves as a consultant and scientific advisory board member to several biotech and venture capital firms. Dr. Sahay was the Chair of the 2018 NanoMedicine and Drug Delivery Symposium (NanoDDS, Portland, OR and CRS Gene Delivery and Editing Focus Group (2020-2021). Dr. Sahay completed his postdoctoral research with Prof. Robert Langer and Prof. Daniel Anderson at the Koch Institute for Integrative Cancer Research at MIT and received his Ph.D. from the University of Nebraska Medical Center under the mentorship of Prof. Alexander Kabanov.

Raymond M. Schiffelers, Ph.D.
Raymond M. Schiffelers is professor of nanomedicine at the UMC Utrecht. He has over 20 years of experience in drug delivery research. His work currently focuses on synthetic and natural nanoparticles to improve diagnosis and therapy. The work in the lab spans fundamental investigations on next generation therapeutics and nanoparticles up to the final stages of nanomedicine development before first-in-man studies.
He focuses in particular on extracellular vesicles in the circulation as inspiration for new drug delivery systems and diagnostic readouts. He is founding member of the International Society for Extracellular Vesicles (ISEV) founding member and member organizing committee for the ISEV2014-annual meeting, Associate Editor of the Journal Extracellular Vesicles and editor of the International Journal of Pharmaceutics and the Journal of Controlled Release. He co-invented OncoCort® a nanomedicine formulation of corticosteroids that entered clinical trials in 2015. He is Founder of EXCYTEX, an extracellular vesicle-based company, and member of the Scientific Advisory Board for a number of start-up companies.
Avi Schroeder, Ph.D.
Avi Schroeder is a tenured Associate Professor of Chemical Engineering at the Technion – Israel Institute of Technology, where he heads the Laboratory for Targeted Drug Delivery and Personalized Medicine Technologies.
Dr. Schroeder conducted his Postdoctoral studies at the Massachusetts Institute of Technology, and his PhD jointly at the Hebrew and Ben Gurion Universities.
Avi is the recipient of more than 30 national and international awards, including named a KAVLI Fellow, the Intel Nanotechnology-, TEVA Pharmaceuticals-, and the Wolf Foundation Krill Awards. Avi is the author of above 50 research papers inventor of 19 patents and co-founder of multiple startup companies based on these discoveries.
Schroeder is a member of Israel Young National Academy of Sciences, Israel’s National Council for Civilian Research and Development, and the President of the Israel Institute of Chemical Engineers.

Robin Shattok, Ph.D.
Robin Shattock has over 30 years’ experience in research and development of vaccines and antiviral therapeutics. He is a Professor of Mucosal Infection and Immunity at Imperial College, London. The focus of his research is the development of vaccines to prevent pandemic threats and poverty related diseases. His publications include over 250 peer-reviewed scientific papers published in a range of peer review journals. Prof. Shattock has led large multi-centre programs funded by the Wellcome Trust, MRC, EPSRC, CEPI, NIH, European Commission, and the Bill and Melinda Gates Foundation. His academic research portfolio includes vaccine projects on SARS-CoV2, HIV, Ebola, Lassa fever, Marburg and Rabies viruses and Chlamydia. He has a strong track record of translation research having taken a wide range of vaccine products through from discovery into clinical testing. The Shattock group was the first in the world to publish on the evaluation of a self-amplifying RNA vaccine against COVID-19 in phase I/II clinical trials. Robin leads the EPSRC Future Vaccines Manufacturing Research Hub at Imperial college. He is Founder of VaxEquity Ltd an Imperial spin-out focused on development of RNA vaccines against human infectious diseases. Robin is an elected fellow of the Academy of Medical Sciences.

Walt Shaw
Fifty-three plus years after founding Avanti Polar Lipids, Inc. Walt Shaw and his partner Rowena retired in August 2020. They remain active, enjoying retirement and have several projects that keep them busy. The most meaningful is developing in collaboration with Young Life organization, Amberjack Farms, a hunting and fishing retreat for young people.

Daniel J. Siegwart, Ph.D.
Dr. Daniel J. Siegwart is an Associate Professor in the Department of Biochemistry and the Simmons Comprehensive Cancer Center (SCCC) at UT Southwestern Medical Center (Dallas, Texas, U.S.A.). He is also the co-director for the Chemistry and Cancer Program within the National Cancer Institute-designated SCCC. He received a B.S. in Biochemistry from Lehigh University (2003), and a Ph.D. in Chemistry from Carnegie Mellon University (2008) with University Professor Krzysztof Matyjaszewski. He also studied as a Research Fellow at the University of Tokyo with Professor Kazunori Kataoka (2006). He then completed a Postdoctoral Fellowship at MIT with Institute Professor Robert Langer and Professor Daniel G. Anderson (2008-2012). He is a co-founder of ReCode Therapeutics. The Siegwart Lab at UT Southwestern aims to discover and define the critical physical and chemical properties of synthetic carriers required for therapeutic delivery of short to long RNAs for gene silencing, delivery, and editing. They have focused on hepatic and extrahepatic delivery for organ and cell specific protein delivery, gene delivery, and gene editing. Their research is grounded in chemical design and takes advantage of the unique opportunities for collaborative research at UT Southwestern.

Gert Storm, Ph.D.
Gert Storm is professor of Targeted Drug Delivery at the Department of Pharmaceutics, at Utrecht University, where he obtained his Ph.D. in 1987. He is also honorary professor (Biomacromolecular Drug Delivery) at the University of Copenhagen and visiting professor at the Department of Surgery of the National University Hospital in Singapore.
Dr. Storm’s major research interests are the design, characterization and (pre)clinical testing of targeted nanomedicine formulations, and the implementation of imaging-guided drug delivery protocols (using e.g. SPECT, MRI, PET).
Over the last decade, clinical translation of academic results has become a vital element of Dr. Storm’s ambition, as exemplified by the clinical development of liposomal corticosteroids (by the creation of the spin-off company Enceladus Pharmaceuticals BV in 2005), the clinical breast cancer study at the University Medical Centre Utrecht (UMCU) evaluating image-guided targeted doxorubicin delivery with hyperthermia (follow-up of the HIFU-CHEM project), his involvement in public-private partnership projects, i.e. EC (coordinator Meditrans (FP6, budget 15M), partnering in 4 FP7 projects and 2 Horizon2020 projects, CTMM (Center for Translational Molecular Medicine, PI HIFU-CHEM project on high intensity focused ultrasound technology to trigger drug release from nanoparticles in tumors), NanoNextNL (National Nanoinitiative, director Program Drug Delivery), TI-Pharma (Top Institute Pharma) and AgentschapNL. Over the years, he also obtained significant funding for applied research from NWO (Netherlands Organisation for Scientific Research) and several large industries (e.g. Astellas, Astra Zeneca, Novartis). He is on the Board of the CLINAM (European Foundation for Clinical Nanomedicine) organization in Basel, Vice-President of the PRC (Phospholipid Research Center) in Heidelberg, Chairman of the Scientific Advisory Board of the Utrecht Centre for Affordable Biotherapeutics (UCAB), Co-Founder of the company Eden Ophthalmic in Singapore, and Scientific Advisor at Liposoma B.V. in Amsterdam.
Since 2014 on, he has been included annually in the lists of The World’s Most Influential Scientific Minds of Thomson Reuters (Highly Cited Researchers), taken over recently by Clarivate Analytics. H-index 115 (Google Scholar May 2022), > 600 publications
Presentation: Therapeutics based on liposomal drug targeting to well-accessible organs | 2:35 pm Tuesday June 14

Ying Tam, M.Sc., Ph.D.
Chief Scientific Officer of Acuitas Therapeutics, Dr. Ying K. Tam, is a globally respected expert in the areas of nanotechnology and immunology. He obtained his M.Sc. and Ph.D. in Developmental and Molecular Biology from the University of Waterloo in Waterloo, ON prior to his post-doctoral fellowship in cancer immunotherapy at the BC Cancer Agency in Vancouver, BC. Dr. Tam has held several academic positions including Instructor and Assistant Professor in the Department of Hematology/Oncology at Rush-Presbyterian-St. Luke’s Medical Center in Chicago, IL, overseeing the translational stem cell transplant immunotherapy research program. He also serves as Adjunct Professor in the Department of Biochemistry and Molecular Biology at the University of British Columbia.
Prior to Acuitas, Dr. Tam led a program developing a lipid nanoparticle (LNP), nucleic acid-based immunostimulatory drug. Dr. Tam is a founding scientist at Acuitas and helped the company to become a global leader in the application of LNP technology for the delivery of nucleic acid therapeutics. This includes the development of the LNP carriers used in Onpattro™ and COMIRNATY®, a highly effective and safe COVID-19 vaccine produced through a partnership with BioNTech and Pfizer.
Dr. Tam oversees the scientific program at Acuitas and has guided both internal research programs as well as external programs with partners and collaborators. He has authored more than 75 peer-reviewed studies, including several in high-impact journals such as Nature and Nature Biotechnology, and has contributed to grant applications to secure millions of dollars in funding.

Presentation: Lipid-based nanopreparations for stimuli-sensitive and organelle-specific targeting | 10:20 am Monday June 13

Alex Torres
Alex Torres is currently the Global Product Manager for the LIPEX® Product Line at Evonik Canada Inc. He has an undergraduate degree in Chemical Engineering from the University of British Columbia. Since joining Evonik in 2014, has had a focus on the LIPEX® extruders, developing equipment for lab-scale to commercial-scale manufacturing.

Peter Van Hoogevest, Ph.D.
Dr. van Hoogevest is Consultant, CEO and Owner at PHARMANOVATION, Rheinfelden (Baden), Germany. He is a pharmacist by training (Utrecht University in The Netherlands), who got his PhD degree in biochemistry 1984 at the Utrecht University in The Netherlands. In 1994 he received the degree of Privatdozent (adjunct professor) in pharmacy at the University of Basel, Switzerland.
His industrial career started at the Biovet Group of the Animal Health Division of Ciba-Geigy Ltd. (Basel) in 1984. Shortly thereafter he obtained a position at the Novel Dosage Form Department of Pharmaceutical Development of the Pharmaceuticals Division of Ciba-Geigy Ltd. After having several positions at this department at Ciba Ltd. and Novartis Ltd. he founded in 1998 together with colleagues of the Pharmaceutical Development Department and reputed industrial managers and scientists the company ADD Advanced Drug Delivery Technologies (Muttenz, CH) and became CEO of this company and was member of the Board of Directors. In 2000 he joined Phares Drug Delivery AG (Muttenz, CH), a company specialized in the delivery of poorly water soluble drug substances, as Managing Director and COO and member of the Board of Directors. From 2012 till 2021 he was Managing Director of the Phospholipid Research Center, Heidelberg and Head of the Scientific Department (including the Development Department) of Lipoid GmbH, Ludwigshafen am Rhein, Germany). He runs from 2021 on his own consulting business PHARMANOVATION, based in Rheinfelden (Baden) , Germany.
His drug delivery expertise, especially in the (phospho)lipid research and development area, is underscored by 78 scientific publications, including 8 book chapters, 33 symposium posters, co-promotion of 48 PhD Theses, 13 patents and 45 patent applications.

Andreas Wagner, Ph.D.
Dr. Andreas Wagner is currently the Head of Liposome Technology at Polymun Scientific GmbH in Klosterneuburg, Austria. He has significant expertise in development and optimization of liposomal drug products. Over the last 15 years, his group guided approx. 15 different liposomal drug products into clinical trials. He studied Biotechnology in Vienna, Austria and earned his Master and Ph.D. degrees in the field of liposomology at the Institute of Applied Microbiology supervised by Prof. Hermann Katinger. Dr Andreas Wagner is listed as inventor on several patents, like the liposome technology and some product patents of liposomal formulations and he has published several peer reviewed articles dealing with liposomes, the technology, products thereof and their application in preclinical and clinical studies.
Presentation: mRNA –vaccines on the fast track – How Polymun contributed to tackling the pandemic | 4:30 pm Sunday June 12

Dominik Witzigmann, Ph.D.
Dr. Witzigmann obtained his Ph.D. in Pharmaceutical Technology from the University of Basel in Switzerland. Following research projects at the University College London (toxicity), German Cancer Research Center (RNAi and cancer), University of Basel (targeted nanomedicines and DNA delivery) and the University of Zurich (mRNA-based genome editing), he joined the team of Dr. Pieter Cullis at the University of British Columbia to focus on extrahepatic RNA delivery utilizing lipid nanoparticle (LNP) systems.
Dr. Witzigmann held leadership roles within the NanoMedicines Innovation Network (NMIN – a Canadian Networks of Centres of Excellence); he co-founded and led NMIN’s NanoCore to support >30 projects with advanced nucleic acid delivery technologies; and he served as a Board Member of the CRS “Gene Delivery and Genome Editing” Focus Group. He has a proven track record in nanomedicines enabling tissue- as well as cell-specific drug and gene delivery.
To translate next-generation LNP technologies into the clinic, Dr. Witzigmann co-founded and leads the LNP-nucleic acid company NanoVation Therapeutics.
Presentation: Next-generation lipid nanoparticle technologies tailored to a variety of tissues | 2:45 pm Sunday June 12

Gang Zheng, Ph.D.
Dr. Gang Zheng is a Professor and Canada Research Chair in Cancer Nanomedicine at the University of Toronto, and the Associate Research Director of the Princess Margaret Cancer Center.
He obtained his BSc in 1988 from Hangzhou University and PhD in 1999 from SUNY Buffalo. Following a postdoctoral training in photodynamic therapy at the Roswell Park Cancer Institute, he joined the University of Pennsylvania in 2001 as an Assistant Professor of Radiology and moved to Canada in 2006.
His lab is best known for introducing the activatable photosensitizers for photodynamic therapy and the porphysome nanotechnology for cancer theranostics. Dr. Zheng is a Fellow of the American Institute of Medical and Biological Engineering and an Associate Editor for Bioconjugate Chemistry.
Presentation: Porphyrin-lipid nanoparticles: building intrinsic multifunction into LNP | 11:10 am Wednesday June 15
Sunday 12 June 2022
10:20 – 11:00 amClinical Opportunities for messenger RNA-LNP Pharmaceuticals
The global success of COVID-19 mRNA-LNP vaccines has validated the clinical utility of this new pharmaceutical modality. In addition, the unique versatility of this platform may allow us to address currently intractable diseases. This presentation will focus on novel mRNA-LNP vaccines and therapeutics currently beginning clinical development or on the immediate clinical horizon.
Sunday 12 June 2022
11:00 – 11:30 am
Therapeutic application of messenger RNA-lipid nanoparticles for in vivo gene editing
Acuitas’ lipid nanoparticle systems (LNP) are enabling clinical development of a range of messenger RNA (mRNA)-based therapeutic approaches including genome editing. The identification and development of editing systems such as CRISPR/Cas9, zinc-finger nucleases and TALENs that precisely edit cellular DNA sequences to stably correct mutated genes and deactivate disease-causing genes has led to a renaissance in gene therapy. The challenge of safe and efficient delivery of editing systems to target cells in the body can be addressed using non-viral LNP-mediated delivery of mRNA encoding the editing enzymes. LNP are able to accommodate the larger nucleic acid payloads often required for editing systems compared to alternative delivery approaches and may also provide potential safety benefits, by avoiding risks associated with viral delivery systems and prolonged enzyme expression to minimize the likelihood of editing at non-target sites. Data demonstrating the ability of intravenously administered mRNA LNP to mediate efficient in vivo editing and exert a pharmacodynamic effect at well tolerated doses in rodents and non-human primates will be presented.
Sunday 12 June 2022
11:30 am – 12:00 pm
Accelerating the Development of Genomic Medicines – Insights into Lipid Nanoparticle Design and Scalable Microfluidic Manufacturing
RNA can be designed and formulated to silence, express, and edit specific genes providing a flexible and powerful approach to preventing and treating diseases. The recent commercialization and widespread distribution of COVID-19 mRNA-LNP vaccines has exemplified the massive potential to rapidly develop and scale-up new genomic medicines to protect from emerging viral threats and treat a wide range of serious diseases with unmet medical needs.
Precision NanoSystems has developed a Genomic Medicine Toolbox for the end-to-end development of RNA-lipid nanoparticles (RNA-LNP). This toolbox comprises an RNA drug substance platform, a nanoparticle delivery platform, and a microfluidics-based nanoparticle manufacturing platform. In this presentation, we provide examples of how these platform technologies are enabling research scientists to rapidly discover new RNA-LNP based vaccines, gene therapies and cell therapies. Furthermore, we will show how Precision NanoSystems can accelerate the development of promising RNA-LNP drug candidates for clinical evaluation and commercialization.
Sunday 12 June 2022
12:00 – 12:30 pm
Tuning lipid nanoparticles for specific applications
Lipid Nanoparticles (LNP) are now well established for delivery of nucleic acids (NA) systemically to hepatocytes and for vaccine applications. However, many potential applications for diverse NA modalities exist outside of these areas. LNP with altered biodistribution can be achieved by changing route of administration, and modulating lipid composition accordingly. This presentation will describe the development of specialized LNP for extrahepatocyte use, with examples including compositions targeting the hepatic stellate cell, lung, muscle and CNS.
Sunday 12 June 2022
1:20 – 1:50 pm
Lipid technology & the race to beat COVID-19
Stephen Burgess, MD, Ph.D. & Walt Shaw
Avanti Polar Lipids has supported and been involved in gene therapy research for over 30 years. Through our manufacturing of high-purity lipids for nucleic acid delivery, we have facilitated clinical development of novel vaccines and therapeutics. We will summarize the path that put Avanti at the forefront of the Race to Beat COVID-19.
Sunday 12 June 2022
1:50 – 2:20 pm
Self-adjuvanting lipid nanoparticle mRNA vaccine for solid tumor immunotherapy
Nucleic acid vaccines, DNA and messenger RNA (mRNA), have emerged as promising modalities for infectious disease and for cancer immunotherapy due, in part, to shortened manufacturing cycles and high potency. Currently, there is limited understanding of the mechanisms of antigen presentation and induction of specific T-Cell responses critical to long-term immunity. Lipid nanoparticles (LNP) composed of ionizable lipids are important components of such vaccines as they can convey and present the nucleic acid effectively to the immune system. Further improvements in LNP carriers require a reduction in the 1) systemic toxicity, 2) improved endosomal escape, 3) potent and T-cell specific adjuvanting function and 4) targeting to specific antigen presenting cells.
Previously we have reported that lipid nanoparticles composed of COATSOME® SS Series can deliver pDNA or mRNA in mice to liver, solid tumors, and other organs via the IV route and achieve high levels of expression. We also evaluated the safety of the lipids in mice where doses of up to 175 mg/kg were well tolerated.
After subcutaneous administration, the LNPs containing an SS-EC, COATSOME® SS Series with vitamin E scaffolds, elicited a higher gene expression activity in comparison with the other LNPs composed of the SS lipids with different hydrophobic scaffolds. Immunization with the SS-EC-LNPs encapsulating mRNA that encodes ovalbumin (OVA, a model antigen) induced both humoral and CTL responses. These findings suggest LNP composed of SS-EC lipid can be effective delivery systems for mRNA vaccines.
Sunday 12 June 2022
2:20 – 2:45 pm
Novel Lipid Excipient Development for the Covid-19 mRNA Lipid Nanoparticle Vaccine
Novel lipid excipients were used to encapsulate RNA within lipid nanoparticles forming the delivery technology behind the Covid-19 vaccine developed by Pfizer and BioNTech called Comirnaty®. Multiple challenges were faced during their development and these challenges along with success factors will be discussed in the presentation.
Sunday 12 June 2022
2:45 – 3:10 pm
Next-generation lipid nanoparticle technologies tailored to a variety of tissues
We are at the most exciting point in human history with respect to the launch and development of nucleic acid therapeutics. In our lifetimes, we will see major diseases including rare genetic, infectious, autoimmune, malignant, and age-related disorders become treatable or even cured. The major issue we currently face is access to state-of-the-art delivery technologies to target diseased tissue safely and effectively. To enable the delivery of nucleic acids to a variety of (extra)hepatic tissues, we have developed a one-stop-shop lipid nanoparticle (LNP) toolbox. NanoVation`s technology portfolio encompasses methods of synthesizing lipids, specialty (ionizable) lipids, LNP compositions, surface-modifying lipids such as PEG-alternatives, as well as mRNA modifications. Our flagship technology, the long-circulating LNP (lcLNP™) platform, enables functional nucleic acid delivery to extrahepatic tissues such as bone marrow, tumors, or skin following intravenous injection. NanoVation`s expertise, platform technologies and services enable partners to rapidly develop their life-changing gene therapies.
This work was supported by an amazing scientific and operational team.
Sunday 12 June 2022
3:30 – 4:00 pm
Advancements in Liposomal Extrusion Technology
The LIPEX® extruder was first introduced to the market in 1985, and quickly became the industry-standard technology for producing liposomal formulations with a uniform particle size population. While proven and effective, the extrusion technology has not seen any major changes or improvements in the extruder design throughout its lifetime.
A major drawback of current extruders and filter membrane holders is the limited area of the filter utilized for extrusion, which causes filter membranes to clog and rapidly foul. This effect is further compounded by a subsequent increase in extrusion pressure that can impact the quality and performance of the final drug product. Frequent and complex filter membrane change during manufacturing is often required to overcome these challenges.
Through 3D computer-aided design, Evonik has now developed an improved membrane support technology to maximize the filter area utilization, significantly reducing back-pressure and filter clogging. This advancement in liposomal extrusion technology addresses process efficiency and product quality, leading to more robust manufacturing processes.
Sunday 12 June 2022
4:00 – 4:30 pm
Phospholipids in Vaccines
Since decades, vaccines and adjuvants using lipid carriers are explored for human and veterinary use. Examples of adjuvants are MF59 and ISCOMs (immune stimulating complexes) as alternative to aluminium salts. Recently, for vaccination against shingles the product Shingrix® of GSK was introduced. This vaccine uses liposomes containing QS21 an immunostimulating saponin as adjuvant. COVID-19 vaccines of Moderna (Spikevax®) and BioNTech/Pfizer (Comirnaty®) use LNPs (Lipid Nano Particles) to deliver mRNA to dendritic cells. Alternatively, liposomes/ISCOMs containing saponins are the adjuvant in the Novavax vaccine for COVID-19 (Novaxavid®). In these vaccines and adjuvants phospholipids are essential excipients.
In this seminar, an overview on the use of phospholipids and their role in vaccines is provided. The phospholipids are discussed with respect to quality and production requirements.
Sunday 12 June 2022
4:30 – 5:00 pm
mRNA-Vaccines on the fast track – How Polymun contributed to tackling the pandemic
Lipid nanoparticles (LNP) are the leading delivery systems for enabling the therapeutic potential of small interfering RNA (siRNA) as well as mRNA for systemic applications. Lipid nanoparticles, currently represent the most advanced platform for RNA delivery, which have now advanced to market products.
During the early days of the Covid-19 pandemic, industry partners reached out to Polymun to set up production processes for mRNA-LNPs together with the respective analytical test methods. Within weeks, a robust and scalable process has been developed, process conditions have been optimized and the process has been adapted to meet requirements for industrial scale. The LNP production process has to meet several requirements, such as simplicity, robustness, potential to scale up and easy handling. Data will be presented, which describe hurdles and solutions throughout these processes.
Sunday 12 June 2022
5:00 – 5:30 pm
AmBisome®: Continued progress & its role in the pandemic
We begin with a review of the historical origins of AmBisome® (liposomal amphotericin B injection) in the Southern California ‘high shear school’ of liposomology that developed a unique platform for liposomal therapeutics with applications to oncology and infectious disease. The formulation and manufacturing principles that co-evolved with the growth in medical application of the drug. Key success factors in manufacturing and scale-up, including the ever tighter needs for aseptic processing quality, and a new parenteral manufacturing facility, will be discussed. Lastly, a mucormycosis fungus epidemic in India, directly related to COVID-19 cases, and the role of AmBisome in that setting, are explored.
Monday 13 June 2022
8:20 – 8:30 am
Liposomes/Lipid Nanoparticles Rule!
Pieter R Cullis, Ph.D., FRSC, FNAI (USA), OC
From their beginnings 60 years ago liposomes and lipid nanoparticles are reaching maturity and are changing the world. It is a time for celebration for all of us in the field. In these opening remarks I will salute the pioneers and suggest we all celebrate our massive success!
Monday 13 June 2022
8:30 – 9:10 am
Lipids, Liposomes and Lipid Nanoparticles: The Past, The Present and The Future
Pieter R Cullis, Ph.D., FRSC, FNAI (USA), OC
I have been working on lipids, liposomes and lipid nanoparticles for a long, long time. Fifty years, to be exact. In this talk I’ll cover some high points from the past, summarize the enormous efforts currently underway that exploit the ability of lipid nanoparticles to enable gene therapies and make some predictions about the future. Exciting times ahead!
Monday 13 June 2022
9:10 – 9:50 am
Species-agnostic in vivo nanoparticle barcoding
RNA can change the expression of any gene, making these molecules promising drugs. However, whether the drug is comprised of siRNA, mRNA, lncRNA, or another nucleic acid, it is limited by one problem: drug delivery. Chemists design thousands of distinct nanoparticles to deliver DNA or RNA to the desired cell type. However, after nanoparticles are synthesized, their ability to deliver drugs is evaluated using in vitro systems devoid of a liver, kidney, spleen, immune system, pulsatile blood flow, and other selection pressures known to affect nanoparticle delivery in vivo.
Here we describe DNA barcoding platforms to quantify how thousands of nanoparticles deliver nucleic acids in vivo. These systems enable us to quantify how hundreds of chemically distinct nanoparticles deliver mRNA or siRNA into up to 30 cell types, all in a single animal. To analyze these large in vivo drug delivery datasets, we have also developed an open source bioinformatics pipeline to iteratively evolve nanoparticles that target cells in vivo. Using this high throughput, iterative, in vivo approach, we have identified nanoparticles with tropism to many novel cell types without the use of active targeting ligands.
This work was supported by the National Institutes of Health and DARPA.
Monday 13 June 2022
10:20 – 10:50 am
Lipid-based nanopreparations for stimuli-sensitive and organelle-specific targeting
Vladimir P. Torchilin, Ph.D., D.Sc.
The efficacy of new generation lipid-based drug delivery systems, such as liposomes, lipid-core micelles, and solid-lipid nanoparticles can be significantly enhanced by providing them with the ability not only to specifically target certain organs or tissues or even individual cells, but also respond in desired way to local physiological stimuli, such as pH, temperature, redox conditions, and overexpression of certain enzymes, but also penetrate cells and deliver active agents to and into individual intracellular organelles. Such multifunctional preparations can be co-loaded with multiple drug combinations as well as combinations of various RNAs with drugs. We have developed several types of liposomes and lipid-core polymeric micelles based on PEG-phospholipid or PEI-phospholipid conjugates, which can firmly bind non-modified or reversibly-modified siRNA and be co-loaded into chemotherapeutic agents. In experiments with cancer cell monolayers, cancer cell 3D spheroids, and in tumor-bearing animals, it was shown that such nanopreparations significantly down-regulate target proteins in cancer cells, enhance drug activity, and reverse multidrug resistance.
To specifically unload such nanopreparations inside target tissues and even in individual cell compartments, we made them sensitive to local stimuli, such as lowered pH, hypoxia, or locally overexpressed matrix metalloproteases. Using pH-, hypoxia-, or MMP2-sensitive bonds between different components of lipid-based nanopreparations co-loaded with siRNA and drugs, we were able to make the systems specifically delivering biologically active agents in required areas as well as to and into individual cell organelles, which resulted in significantly improved therapeutic response.
Monday 13 June 2022
10:50 am – 11:20 pmMultifunctional Envelope-type Nano Device from Controlled Intracellular Trafficking to Clinical Application for Nanomedicines
We are developing a multifunctional envelope-type nano device (MEND) as a novel non-viral gene delivery system based on a new packaging concept termed “Programmed Packaging”.
Cytosolic delivery: MEND was modified octaarginine (R8) to enhance cellular uptake and GALA peptide was also introduced to enhance endosomal escape. The R8/GALA-MEND can deliver siRNA successfully to dendritic cells (DC) to increase immune response, however, the antitumor activity was not sufficient. Then we introduced newly designed pH-sensitive cationic lipid YSKC12 and YSKC12-MEND can induce remarkable silencing effect in human NK cells as well as DC and T-cells.
In vivo delivery: In order to apply MEND via a systemic administration, we designed a pH-responsive cationic lipid to control biodistribution as well as intracellular trafficking. A newly designed YSK05 can respond to endosomal pH to induce efficient escape from endosome while maintaining neutral surface charge in blood circulation. The YSK-MEND can induce gene silencing in hepatocytes at a dose of 0.06 mg/kg. YSK-lipids were optimized based on chemical library which contains diversified chemical structures of YSK-lipids. The most efficient delivery of siRNA has been achieved by CL4H6 of ED50 at 0.0025 mgsiRNA/kg for gene silencing in hepatocytes in vivo after iv administration. Application of a new pH-sensitive cationic lipids for genome editing will be discussed.
Mitochondrial delivery: We proposed a MITO-Porter, a liposome-based carrier system that introduces macromolecular cargos into mitochondria via membrane fusion manner. An antisense RNA oligonucleotide (ASO) against cytochrome c oxidase subunit II was encapsulated into MITO-Porter to knockdown mitochondrial RNA. MITO-Porter can successfully knockdown the targeted mitochondria-encoded mRNA, protein and membrane potential in HeLa cells. D-arm, a mitochondrial import signal of tRNA to the matrix was chosen as ASO. Mitochondrial gene therapy will also be discussed based on our recent data in mutated human cells.
Monday 13 June 2022
11:20 – 11:50 am
Polymer/Oil-Based Nanocapsules vs. Lipid Nanoparticles as RNA Delivery Vehicles
Our laboratory started the development of polymer-based nanocarriers for the delivery of polynucleotides in the late 90’s. We first produced PLGA-PEG nanospheres for the delivery of DNA and then, moved to cationic polymer (chitosan, polyarginine and protamine) -based nanocarriers, which were intended for different therapeutic purposes going from ocular drug delivery to vaccination and immunotherapy. The role of the cationic polymers was not only to condense the polynucleotides but also to facilitate their transport across biological surfaces. More recently, in the context of the B-SMART EU project, we developed strategies to deliver RNA to the brain. The nose-to-brain delivery prototype involves the combination of a penetration enhancer (C12-modified-octarginine) and a protective polymer (polyglutamic acid-PEG), whereas the one intended to cross the brain-blood barrier (BBB) through systemic administration is a ligand-functionalized oil-based nanocarrier. Finally, we have also contributed to the knowledge about mRNA vaccination. More precisely, we have developed a series of more than 300 prototypes of polymer/oil-based nanocapsules and lipid nanoparticles. A selected library of prototypes with adequate physicochemical properties was analyzed in terms of their transfection efficacy using model RNA and immunogenicity with a COVID RNA candidate. The overall conclusion was that not only the components but also their structural organization were key for their performance. An immense landscape for the optimization of RNA delivery is now open.
This work was supported by European Union’s Horizon 2020 research and innovation program (grant agreement No. 721058), MINECO- PCIN-2017-129/ AEI (EuroNanoMed III), Instituto Salud Carlos III, FEDER Funds, Ref. COV20/00214.
Monday 13 June 2022
12:50 – 1:20 pm
On the mechanism of tissue-specific mRNA delivery by selective organ targeting (SORT) lipid nanoparticles (LNPs)
Lipid nanoparticles (LNPs) are a clinically mature technology for the delivery of genetic medicines but have limited therapeutic applications due to liver accumulation. Recently, our laboratory developed selective organ targeting (SORT) nanoparticles that expand the therapeutic applications of genetic medicines by enabling delivery of messenger RNA (mRNA) and gene editing systems to non-liver tissues. SORT nanoparticles include a supplemental SORT molecule whose chemical structure determines the LNP’s tissue-specific activity. To understand how SORT nanoparticles surpass the delivery barrier of liver hepatocyte accumulation, we studied the mechanistic factors which define their organ-targeting properties. We discovered that the chemical nature of the added SORT molecule controlled biodistribution, global/apparent pKa, and plasma protein interactions of SORT nanoparticles. Additionally, we provide evidence for an endogenous targeting mechanism whereby organ targeting occurs via 1) desorption of poly(ethylene glycol) lipids from the LNP surface, 2) binding of distinct proteins to the nanoparticle surface because of recognition of exposed SORT molecules, and 3) subsequent interactions between surface-bound proteins and cognate receptors highly expressed in specific tissues. These findings establish a crucial link between the molecular composition of SORT nanoparticles and their unique and precise organ-targeting properties and suggest that the recruitment of specific proteins to a nanoparticle’s surface can enable drug delivery beyond the liver.
Monday 13 June 2022
1:20 – 1:50 pm
Boosting intracellular delivery of mRNA therapeutics and its applications
The field of nanomedicine is moving from an age of renaissance towards industrial revolution. In part due to the transformational impact of lipid nanoparticle (LNP) enabled mRNA vaccines against SARS-CoV2. Our lab has worked extensively onto understanding LNP design, structure, and its impact on intracellular delivery of mRNA. Endosomal sequestration of LNPs remains a formidable barrier to intracellular delivery. Structure-activity analysis of cholesterol analogues reveals that incorporation of C-24 alkyl phytosterols into LNPs (eLNPs) causes 200-fold improvement in gene transfection and the length of alkyl tail, flexibility of sterol ring and polarity due to -OH group is required to maintain high transfection. Cryo-TEM displays a polyhedral shape for eLNPs compared to spherical LNPs, while x-ray scattering shows little disparity in internal structure. eLNPs exhibit higher cellular uptake and retention, potentially leading to a steady release from the endosomes over time. 3D single-particle tracking shows enhanced intracellular diffusivity of eLNPs relative to LNPs, suggesting eLNP traffic to productive pathways for escape. Based on these findings we designed next generation LNPs for deliver mRNA for extrahepatic gene delivery and editing i.e., for the treatment of cystic fibrosis, retinal degeneration, and COVID-19 therapeutics. I will also discuss our recent data on delivery of LNPs delivered mRNA in non-human primate eye. Our findings emphasize the need for greater insights into surface topology and structural properties of nanoparticles, and their subcellular interactions. Next generation LNPs that enable tissue and cell-type specific delivery of genes and genome editors can revolutionize modern medicine.
Monday 13 June 2022
1:50 – 2:20 pm
Development of broadly protective influenza vaccines using nucleoside-modified mRNA
Influenza virus is one of the most important human pathogen. The influenza mortality is estimated to be approximately 650,000 per year worldwide, in addition, occasional global pandemics can infect up to 20-40% of the world’s population. Licensed influenza virus vaccines require annual reformulation and readministration due to poor IgG longevity and lack of neutralization of related viruses. Development of a universal influenza virus vaccine with the potential to elicit long-lasting, broadly cross-reactive immune responses is necessary for reducing influenza virus prevalence. We have utilized lipid nanoparticle-encapsulated, nucleoside-modified mRNA vaccines to deliver a combination of influenza A group 1 or influenza B antigens to induce strong immune responses with substantial breadth and potency in a murine model. A single immunization with 50 ng of combined influenza A group 1 or combined influenza B vaccines induced protective immune responses against a broad panel of group 1 or influenza B viruses, respectively. These findings support the advancement of nucleoside-modified mRNA-lipid nanoparticle vaccines expressing multiple antigens as universal influenza virus vaccine candidates.
Monday 13 June 2022
3:00 – 3:30 pm
Army Liposome formulation with QS21 (ALFQ): A potent & safe vaccine adjuvant
Addition of the triterpenoid saponin QS21 to nano-sized saturated phospholipid liposomes containing >50 mol% cholesterol (when compared to the phospholipids), and also containing monophosphoryl lipid A (MPLA), results in the formation of ALFQ, which contains unilamellar vesicles as large as 30 microns. This process occurs by a remarkable fusion event in which nanoliposomes are transformed spontaneously into micro-liposomes. When compared with the composition of Adjuvant System 01 (AS01, GSK), a liposomal adjuvant present in two licensed vaccines (Shingrix® and Mosquirix®), ALFQ differs as follows: AS01 contains unsaturated phospholipid (e.g., DOPC ) as the bulk lipid, but ALFQ contains DMPC and DMPG; AS01 contains 30 mol% cholesterol, but ALFQ contains >50% cholesterol; AS01 contains 50-100 nm particles but ALFQ is a polydisperse suspension of particles ranging from 50-30,000 nm. Despite polydispersity, nearly all of the ALFQ particles, in terms of total volume and surface area, are pelleted by centrifugation at 12,000 x G; in contrast, none of the nanoliposome particles are visibly pelleted by similar centrifugation. To date, three experimental vaccines adjuvanted by ALFQ, two malaria vaccines and a SARS-CoV-2 vaccine, have completed phase 1 clinical trials, and have been deemed safe. Potency results are pending. Five additional phase 1 trials with ALFQ adjuvant, three candidate HIV-1 vaccines, a Campylobacter diarrhea vaccine, and a universal influenza vaccine with unconjugated peptides as antigens which has shown promising results in a relevant animal model, are approved by WRAIR or other sponsors, and all are in various stages pending initiation.
Monday 13 June 2022
3:30 – 4:00 pm
Optimization of lipid nanoparticles for self-amplifying RNA expression & cellular
activation using a design-of-experiment approach
Lipid nanoparticles (LNPs) are the leading technology for RNA delivery, given the success of the Pfizer/BioNTech and Moderna COVID-19 messenger RNA (mRNA) vaccines, and small interfering RNA (siRNA) therapies (patisiran). However, optimization of LNP process parameters and compositions for larger RNA payloads, such as self-amplifying RNA (saRNA), which can have complex secondary structures, have not been performed. Furthermore, the interactions between process parameters, critical quality attributes (CQAs) and function, such as protein expression and cellular activation, are not well understood. Here, we used two iterations of Design of Experiments (DoE) (Definitive Screening Design and Box Behnken Design) to optimize saRNA formulations using the leading, FDA-approved ionizable lipids (MC3, ALC-0315 and SM-102). We observed that PEG is required to preserve the CQAs and that saRNA is more challenging to encapsulate and preserve than mRNA. We identified three formulations to minimize cellular activation, maximize cellular activation or meet a CQA profile while maximizing protein expression. These compositions and parameters may be useful for designing formulations for a range of applications, such as vaccines or protein replacement therapies, for larger RNA cargoes.
Monday 13 June 2022
4:00 – 4:30 pm
LNP formulated saRNA – learning from clinical experience
Lipid nanoparticle (LNP) encapsulated self-amplifying RNA (saRNA) is a novel technology with significant, and previously untested, potential for translation into human use in the development of novel drugs and vaccines. Vaccines against COVID-19 require production technology that is highly scalable to meet global demand. Vaccines developed using encapsulated saRNA have unique features, which include low dose administration and a readily modifiable antigenic domain making it possible to formulate vaccines rapidly. As part of the global effort to develop novel SARS-CoV-2 vaccines we took an saRNA vaccine from an early design concept through to clinical evaluation. Early preclinical evaluation demonstrated potent anti-SARS-CoV-2 immunogenicity in small animals even at ultra-
low doses (0.01μg) and efficacy against infection in guinea pig challenge studies. However, while LNP formulated saRNA was seen to be safe and well tolerated, human responses to SARS- CoV-2 were significantly lower than those predicted by small animal models, failing to provide seroconversion in 100% of participants. Retrospective analysis of the predictive nature of different animal models and improved understanding species specific differences in innate regulation of saRNA expression are providing critical insight to improved vector design, LNP formulation and development of better preclinical models. This presentation will provide learnt experience form our clinical development program with a view to future improvements and challenges for LNP formulated saRNA.
Monday 13 June 2022
4:30 – 4:50 pm
The development of effective medicinal products in Africa by Africa for Africans
More than one-sixth of the world’s population are infected with at least one neglected tropical disease (NTD), with an additional two billion people at risk, resulting in more than 185,000 fatalities annually. The WHO lists 18 NTDs that not only affect health, but also the economic prosperity and often the very survival of poor and marginalized communities in regions of Africa, Asia and Latin America, and consequently the achievement of the declared global Sustainable Development Goals (SDGs) is also at risk. Six of the NTDs can be controlled or even eliminated through mass administration of medicines or control of the carrying vector or other effective interventions, but treatment of the other 12 NTDs presents with low efficacy due to drug resistance, short half-life, toxic side effects, and low bioavailability – the development of combat strategies against these 12 diseases in particular requires urgent attention.
Covid-19 vaccine, by demonstrating the effectiveness of vaccine strategies to curb endemic disease spread, has elevated public support for science and created an opportunity for scientists to investigate cures / treatments for infectious diseases in general, including the NTDs. It also points to the safety of nano-delivery systems. Hence we are, for the first time in history, seeing an increase in support for African vaccine manufacturing and transfer of skills by the pharmaceutical industry, with the large Covid-19 vaccine manufacturers setting up modular manufacturing facilities in a number of African countries. Indeed, there is increased interest in developing improved research capabilities, and novel drug delivery systems, in Africa. As illustration, this talk will include some results of (i) preclinical studies of a SARS-CoV-2 vaccine with the potential to be effective, efficient, including for the delta-variant and (ii) the use of a South African developed nano-delivery system in preclinical and clinical studies for various infectious diseases.
The development of vaccines for Africa by Africans has become a favourite slogan of politicians; hopefully this can translate into reality with the strengthening of continental expertise in scientific, regulatory and manufacturing disciplines. The local production of vaccines and medicines that are safe, effective, affordable and accessible will reduce the dependence of this continent on imported medicinal products, it will help to ensure medicinal product security, and will support much needed economic growth in Africa.
Tuesday 14 June 2022
8:30 – 9:10 am
Lipid nanoparticles for overcoming biological barriers to mRNA delivery
Significant advances have been made in the development of messenger RNA (mRNA) therapeutics for vaccine, protein replacement, and gene editing applications. However, these therapeutics must overcome numerous obstacles to be successful, including rapid in vivo degradation, poor uptake into target cells, required nuclear entry, and potential in vivo toxicity in healthy cells and tissues. In this talk, I will discuss our efforts towards the development of new lipid nanoparticles (LNPs) that enable the delivery of mRNA to target cells and tissues in vivo. I will describe new therapeutic strategies utilizing these LNPs for (i) mRNA CAR T cell engineering for cancer immunotherapy, and (ii) in utero mRNA delivery for treating disease before birth.
Tuesday 14 June 2022
10:30 – 11:00 am
Overcoming the barrier – Topical gene therapy of skin & lung
Bleeding and thrombotic disorders are common, affecting hundreds of thousands of North Americans, often due to an imbalance between the formation (coagulation) and destruction (fibrinolysis) of blood clots. Modulating fibrinolysis instead of coagulation is an alternate clinical approach for patients with bleeding and thrombotic disorders. However, there are only a small number of medications that influence pro- and anti-fibrinolytic proteins and enzymes, and they are short-acting. We developed a library of siRNA and lipid nanoparticle (LNP) agents targeting pro- and anti-fibrinolytic proteins to modulate fibrinolysis long-term. Encapsulating siRNA agents in LNPs enables delivery to the liver, where many pro- and anti- fibrinolytic proteins are synthesized. siRNA mediates gene silencing by degrading the target mRNA, resulting in long-term depletion of the corresponding protein in blood plasma for weeks to months. Administering pro- and anti-fibrinolytic siRNA-LNPs effectively modulated fibrinolysis in vivo for weeks to months. In small and large animal models of bleeding and thrombosis, the appropriate siRNA-LNPs corrected bleeding or thrombosis, showing promising therapeutic potential for humans.
Tuesday 14 June 2022
11:00 – 11:30 am
Overcoming the barrier – Topical gene therapy of skin & lung
Epithelia such as human skin or human lung are a highly interesting target for the delivery of a great variety of biomacromolecules including biologicals, siRNA, and gene editing tools such as CRISPR. In fact, the main limitation that currently hampers broad clinical translation, especially of gene therapies is the lack of safe and efficient delivery strategies.
As epithelia are the first defense line of the human body, they developed a variety of very effective protective mechanisms. As such, the absorption of molecules across the skin is limited to small and moderately lipophilic substances due to the unique composition and, hence, very tight barrier of the stratum corneum. Lung epithelium instead is covered by a mucus gel which also greatly hampers efficient penetration of especially biomacromolecules. For both, however, applying drugs topically appears to be the only viable option when targeting the epithelial cells or basal cells of these tissues.
In this presentation, I will discuss the potential of lipid nanoparticles as delivery systems for gene delivery to human epithelia and will allude to the remaining challenges in this field.
Tuesday 14 June 2022
11:30 am – 12:00 pm
Optimizing lipid nanoparticles for in vivo therapeutic genome editing
Genetic diseases are a leading cause of death and disability in Canada with immense economic and societal burdens. Gene therapy has emerged as a means to effectively treat genetic diseases; however, current gene therapies are limited by their high manufacturing costs, the inability to re-dose, and the safety concerns of some viral vectors. CRISPR genome editing is a new therapeutic approach that aims to directly repair the underlying disease-causing mutations. Conventional CRISPR methods are limited as in vivo therapeutics because they introduce DNA breaks and cause frequent off-target edits. Newer base editors and prime editors overcome the limitations traditional CRISPR genome editing methods because they do not introduce DNA breaks. However, the delivery of genome editors to affected tissues remains a challenge. Viral vectors, such as AAV, are unsuitable because their long expression (years) increases the probability of unintended edits. In contrast, the transient expression (hours-days) of RNA encoding genome editors via nanoparticles is well suited for genome editing, and unlike viral vectors, nanoparticles can be readministered. However, nanoparticle delivery of complex genome editing cargos (large mRNA + small gRNA) remains a challenge, especially to extra-hepatic target tissues such as muscle. To address this, we are developing new ways to safely deliver these new editors using lipid nanoparticles. To efficiently measure the in vivo effectiveness of genome editor delivery via LNPs, we have developed transgenic mice that carry mutations in reporter genes. Precise gene repair of these mutations produce a functional enzyme that emits light (luminescence) that sensitive imagers can detect to precisely measure the location and extent of gene editing in living animals. We have made progress in our goal towards efficient and safe in vivo genome editing that we will share.
Tuesday 14 June 2022
1:05 – 1:35 pm
Translational models to evaluate the performance of lipid based delivery systems
The transition from nanoparticle design to in vitro assessment and finally in vivo experiments in higher vertebrates remains a challenge. Phenomena such as protein binding, cellular uptake and intracellular processing are of prime importance since they may have a strong impact on biodistribution and immunogenicity of nanoparticles. Therefore, particle characteristics should be studied in an environment that simulates the situation encountered in biological systems. We will discuss the use of zebrafish (Danio rerio) larvae as a vertebrate screening model to assess the systemic circulation and extravasation of lipid-based drug delivery systems in vivo. To validate this novel approach, monodisperse preparations of fluorescent labelled liposomes with similar size and zeta potential were injected into transgenic zebrafish lines expressing green fluorescent protein in their vasculature. Phosphatidylcholine based lipids differed by fatty acid chain length and saturation. Circulation behaviour and vascular distribution pattern were evaluated qualitatively and semi-quantitatively using image analysis. The circulation patterns in the zebrafish model did correlate with published and experimental pharmacokinetic data from mice and rats. Our findings indicate that the presented translational approach can be used to predict the in vivo performance of lipid based delivery systems.
Tuesday 14 June 2022
1:25 – 1:45 pm
Targeted liposomal drug delivery to pediatric sarcomas
We are developing liposomes targeted to the tumor site to improve current therapies for pediatric sarcomas. The high relapse rates together with the significant toxicity, generating late side effects, caused by the aggressive chemotherapies needed to fight relapsed tumors, are major complication in pediatric oncology. Peptides and nanobodies with strong affinity for rhabdomyosarcoma (RMS), the most common soft tissue sarcoma in children, were selected and tested. In vitro binding of liposomes to RMS could be dramatically increased. The in vivo efficacy is under evaluation in an orthotopic model of RMS.
Tuesday 14 June 2022
1:45 – 2:05 pm
Lipid Self-Assembling Nanoparticle for RNA Delivery: Toward Personalized Medicine
Lipid self-assembling nanoparticles (SANPs) represent a promising platform for RNA delivery. RNA can be loaded before use, thus paving the way for a personalized medicine. Different applications of SANP for RNA delivery will be presented.
Tuesday 14 June 2022
2:05 – 2:35 pm
Liposomal Hydroxychloroquine-An example of what can happen
to a liposomologist during the COVID pandemic
Hydroxychloroquine (HCQ) is an approved anti-malarial drug that has the potential to be repurposed for cancer indications. Preclinical studies found that HCQ can improve the anti-cancer effects of various therapeutic agents by impairing autophagy. These findings are difficult to translate in vivo as reaching an effective concentration of HCQ is challenging. Dose escalation is not sufficient, as HCQ is cardiotoxic. We developed liposomal formulations of HCQ that were capable of increasing the plasma circulation lifetime of HCQ. Pharmacokinetics analysis of plasma samples derived from CD1 mice showed that both formulations engendered ~850-fold increases in total drug exposure over time relative to free drug. An efficacy study carried out with liposomal or free HCQ in combination with the gefitinab (an Epidermal Growth Factor Receptor (EGFR) inhibitor) which induces autophagy, showed that liposomal HCQ provided therapeutic benefits when tested in immunocompromised mice bearing gefitinib-resistant JIMT-1 breast cancer tumor xenografts. Western blot analysis of JIMT-1 tumor tissue harvested from animals at the end of treatment showed that the liposomal HCQ and gefitinib combination augmented inhibition of autophagy in vivo as demonstrated by increased LC3-II and p62/SQSTM1 (p62) protein expression compared to free HCQ combination. Our results suggest that liposomal HCQ modulates autophagy in vivo. But stop the press- the COVID-19 pandemic came and what does one do when it is dictated that cancer research studies need to be put on hold? Well it turns out liposomal HCQ could be repurposed for treatment of SARS CoV2 infections- and when opportunity knocks… But hold the press – Donald Trump has something to say!
Tuesday 14 June 2022
2:35 – 3:05 pm
Therapeutics based on nanoparticulate drug targeting to well-accessible organs
In the healthy body situation, the overwhelming majority of systemically administered nanoparticles will end up in the liver and the spleen. Other organs and tissues are not or hardly reached due to the presence of the vascular endothelium barrier. Then only local administration would be an option, though this is only possible in a limited number of cases. These excellent targeting opportunities are known for decades, but nanoparticle-based therapeutic products for treating patients suffering from pathologies associated with these well-accessible organs are still largely lacking, with the recent Onpattro product targeting siRNA to hepatocytes (i.v. administration) and Covid-19 mRNA vaccins (i.m. administration) being recent exceptions. In this talk, I will present our ongoing efforts to exploit the spontaneous passive behaviour of nanoparticles for the development of new therapeutics. Topics will include: targeting to the eye to treat eye inflammation (1), targeting to liver to treat fatty liver (2) and targeting to the spleen to treat cancer (3).
Ongoing collaborations exist with:
1. Prof. Dr. Tina Wong and Dr. Chee Wai Wong (Singapore National Eye Centre (SNEC), Singapore Eye Research Institute (SERI)) and Dr. Bart Metselaar (Liposoma BV, Amsterdam Science Park, and Laurentia Holding, Naarden, The Netherlands))
2. Dr. Ruchi Bansal and Prof. Dr Jai Prakash (Advanced Organ Boengineering and Therapeutics, University of Twente (UT)) and Dr. Jiong-Wei Wang, Dr. Giorgia Pastorin and Prof Dr. Lee Chuen Neng (Surgery, Pharmacy, National University of Singapore) (NUS)) and Dr. Ruchi Bansal and Prof. Dr Jai Prakash (Advanced Organ Boengineering and Therapeutics, University of Twente (UT))
3. Dr. Joke den Haan, Prof. Dr. Yvette van Kooyk, PhD Maarten K Nijen Twilhaar (Molecular Cell Biology and Immunology, Amsterdam University Medical Center (Amsterdam UMC) and PhD Lucas Czenter and Dr. Cornelis van Nostrum (Pharmaceutics, Utrecht University) (UU))
Tuesday 14 June 2022
3:05 – 3:45 pm
Nanomedicine quo vadis? Lessons learned as scientist, developer & entrepreneur
Yechezkel (Chezy) Barenholz, Ph.D.
LRD 2022 should be a celebration of the great success of Nanomedicine and nano-drugs as the BioNTech/Pfizer and Moderna mRNA-LNP vaccines saved a large percentage of world population from the COVID-19 pandemic. The success of these vaccines stems from three independent factors: The first one is the sound basic science leading to the development of modified mRNA with improved stability and reduced immunotoxicity; as well as to the parallel development of the LNP based on ionizable cationic lipids and PEG lipids that serve as an efficient delivery system of this mRNA. Upon intramuscular injection the desired mRNA is reaching the immune and muscle cell’s cytoplasm. This allowed (without the need to reach cell nuclei) the expression of the protein encoded by the mRNA (Spike protein), leading to trigger of the immune response that protects the vaccine recipient against the infectious virus.
Second factor is the development of a “huge”-(kg)-scale “Good Manufacturing Production” (GMP) of relevant modified mRNAs suitably modified to improve their stability and reduce their immunotoxicity.
The third factor is the development and scale-up of the synthesis at GMP level of unique lipids and lipid compositions which, when combined with the relevant mRNA, are producing the highly efficacious mRNA-LNPs vaccine at a huge-scale of 100th of litters under GMP conditions. The successful combination of these three factors enables the production and the clinical use of billions of efficacious vaccine doses. Therefore, it seems that many of the technological obstacles to the development of nano-liposome and LNP based drug products were overcome.
However, despite this great progress, and the FDA approval of almost 10 nano-drugs, the clinical therapeutic success of nano-drugs and nanomedicine remain limited by biological, and immunological barriers. The reasons are related to the large differences between the desired activity of preventative locally (IM) administered vaccines and therapeutic use of other liposomal/LNP based drug products which in most cases are administered systemically and at much higher levels than the vaccines. It is expected of these drug-products to reach the relevant disease sites. To overcome these obstacles there is a need that the Nanomedicine community will join forces and apply a multidisciplinary- approach based on bio-convergence. Firstly, we must identify the mechanisms that are the basis for barriers to optimal nanomedicine and only then to develop the means to overcome these obstacles, so nano drugs can meet their expectations. This requires focusing on physicochemical, biological, toxicological, immunological, and translational factors and the understanding the crosstalk between these factors.
Tuesday 14 June 2022
4:15 – 4:55 pm
100 Years of Vaccine Science
The history of vaccination is a testament to the continuity of science, building on decades of knowledge to find truth, develop consensus, and solve problems for the greater good. The origin of vaccination goes back more than 1000 years when variolation – the administration of human pus from smallpox blisters – was practiced to reduce the consequences of smallpox infection. The smallpox virus in the pus is attenuated by the immune response from the donor. In 1798 Edward Jenner recognized that pus from cowpox infected cows can be administered safely to humans to induce protective immunity against smallpox in humans. “Vaccine Farms” were established worldwide to harvest cowpox virus from blisters on the flank of cows, produce enough attenuated virus to vaccinate everyone on earth, and rid the world of smallpox in 1977.
During his lifetime Luis Pasteur developed “Germ Theory” discovering microorganisms that are the cause of numerous infectious diseases. In 1880 Pasteur discovered that attenuated microorganisms could be propagated in the lab and used for vaccination – he predicted that this would rid the world of infectious disease. It wasn’t until finally in 1935 that attenuated Yellow Fever virus vaccine, grown in embryonic chicken eggs was introduced. The next 20 years was the hay day in vaccine development when polio (Sabin/Salk) and 9 other attenuated organism vaccines (Hilleman) were introduced that are still manufactured today in similar antiquated, laborious, and hazardous ways.
In 1993 Maurice Hilleman from Merck threw his support into the field of nucleic acid vaccines calling it, “… one of the most exciting things in modern vaccinology”. Nucleic acid sequences could be administered repeatedly without mounting an immune response against the vector. Manufacturing of plasmid DNA was reproducible and scalable, a modern agile approach to immunize against different encoded proteins and thus protect against a variety of diseases. Much clinical development in nucleic acid immunization was accomplished since then but success never reached the pinnacle it has today. This is largely because of the challenging cancer and viral targets that were prioritized then and because we lacked the spectacular lipid nano particles available today. Through the combined efforts of many. we’re finally at the dawn of this new modality, “… one of the most exciting things in modern vaccinology.”
Wednesday 15 June 2022
8:30 – 9:10 am
Complexity & Reality: The Case of Thermosensitive Liposomes
Over the past few years there have been many articles debating the value of nanomedicines. To date, nanomedicines in oncology have largely resulted in improvements in the toxicity profile of drugs with few leading to enhancements in therapeutic outcomes relative to standard of care. There also continues to be a discrepancy between pre-clinical and clinical success of nanomedicines that may in part be attributed to a prioritization of novelty over innovation. Drug formulation development should be pursued from the outset with a focus on the patients’ needs as well as translational feasibility (i.e. scale-up and manufacturing, economic feasibility and competitive landscape). As a case study, I will discuss thermosensitive liposomes, with a specific focus on the pre-clinical development and clinical evaluation of ThermoDox. I will also share studies from our laboratory on the design of new formulations that provide localized delivery of drugs when combined with clinically relevant heating modalities.
Wednesday 15 June 2022
9:10 – 9:40 am
Lipid nanoparticles for cancer immunotherapy
The current standard of care for peritoneal metastases of cancer includes cytoreductive surgery and chemotherapy, but the treatment response varies among patients with a high recurrence rate. My lab explores using lipid nanoparticles (LNPs) to regionally activate the immune system to promote immune clearance of peritoneal metastases. It was demonstrated that cationic LNPs displayed increased peritoneal retention compared to the neutral and anionic LNPs. R848, a TLR7/8 agonist, delivered by the cationic LNPs showed increased accumulation in the peritoneal fluid and peritoneal immune cells, but delayed absorption to the systemic circulation compared to free R848. This led to elevated levels of IFN-alpha in the peritoneal fluid but not plasma in the LNP-R848 group. Mice with intraperitoneal metastases of CT26 colon cancer cells were first treated with oxaliplatin followed by LNP-R848, and 60-70% of the mice were cured, compared to a 30% cure rate when treated with oxaliplatin + free R848, and 0% cure rate when treated with oxaliplatin + PBS. These cured mice became immunized against the same tumor in a tumor re-challenge study. Re-exposure of tumor antigens to their splenocytes induced CD4 and CD8 proliferation and secretion of IFN-gamma. The results confirmed that the therapy with LNP-R848 induced specific antitumor immunity in the mice, leading to immune clearance and cure of the disease.
Wednesday 15 June 2022
9:40 – 10:10 am
Enhancing T cell functionality with nanotechnology in adoptive cell therapy
The development of our understanding of the immune system has resulted in many new avenues for nanotechnology including use of liposomes and lipid nanoparticle systems (LNPs) to alter the function of T cells in relation to adoptive T cell therapy. Therapeutically succesful adoptive T cell therapy is dependent on effective gene engineering of TCR or CAR targeting proteins, gene editing or other functional modifications to enhance T cell function to overcome barriers to engraftment as well as making the T cells resistant to premature exhaustion. Combing adoptive cell therapies with LNP based vaccines is another avenue for using lipid nanotechnology to enhance therapeutic outcome. Our research has in recent years been focused on various methodology for using lipid nanotechnology to enhance the efficiency of T cell therapy in cancer treatment, which will be presented.
Wednesday 15 June 2022
10:40 – 11:10 am
The PEG-mediated accelerated blood clearance effect in mRNA-LNP evoked T-cell immunity
Lipid nanoparticles (LNPs) are currently at the forefront for the delivery of nucleic acid therapeutics, as exemplified by patisiran and the COVID-19 vaccines. We made a library of lipid nanoparticles loaded with mRNA and measured physicochemical characteristics. In vivo tissue distribution was determined after intravenous administration in mice using fluorescent RNA payloads and correlated to functional tissue distribution determined by reporter protein expression. Finally, therapeutic immunogenic mRNA payloads were used to examine the magnitude of an antigen-specific T cell response. From these data a model was built to correlate LNP composition to efficacy. Based on the model a suboptimal and optimal composition was established to validate the model. These compositions were tested for antitumor activity, which demonstrated strong antitumor activity of the optimal LNP composition and validated the model. Crucial cell types for activity were macrophages, monocytes and dendritic cells that likely acted as antigen presenting cells. In addition, Interferon I signaling was crucial for CD8 antigen-specific T cells. Upon repeated injection anti-PEG antibodies were formed that did not preclude induction of a specific T cell response.
This work was supported by grant 16169 TORNADO of the Netherlands Organization for Scientific Research.
Wednesday 15 June 2022
11:10 – 11:40 am
Porphyrin-lipid nanoparticles: building intrinsic multifunction into LNP
Porphyrins are light-absorbing molecules clinically used for photodynamic therapy and fluorescence imaging. Conjugating porphyrin to lysophospholipid forms porphyrin-lipid, a building block molecule that self-assembles into a liposome-like nanoparticle called porphysome. These simple porphyrin-lipid building blocks impart inherent multifunctionality to LNP for unparalleled theranostic utility (e.g., photothermal, photoacoustic, photodynamic, fluorescence, PET, MRI, and drug delivery). Using the same building blocks, we also created a large family of porphyrin-lipid nanoparticles with different sizes, shapes, and functions. Replacing porphyrin-lipid with other dye-lipid analogues such as texaphyrin-lipid resulted in nanotexaphyrins, a new class of radiotheranostic nanomedicine capable of alpha, beta and Auger electron therapies. The simple, intrinsically theranostic nature of the porphyrin-lipid nanoparticles epitomizes a “one-for-all” nanomedicine design paradigm and confers exciting clinical promise.
This work was supported by TFRI PPG, CIHR, OICR CATA, CCSRI, NMIN, CFI, Canada Research Chair Programs, and Princess Margaret Cancer Centre
Wednesday 15 June 2022
11:40 am – 12:10 pm
The role of mRNA delivery system and route of administration on vaccine potency
The efficacy of RNA-based vaccines has been recently demonstrated, leading to the use of mRNA based COVID-19 vaccines delivered using lipid nanoparticles. To investigate the impact of different nanoparticle delivery platforms and administration routes on RNA-vaccine potency, we investigated the immunogenicity of a self-amplifying mRNA encoding the rabies virus glycoprotein encapsulated in different nanoparticle platforms (solid lipid nanoparticles (SLNs), polymeric nanoparticles (PNPs) and lipid nanoparticles (LNPs)). These were administered via three different routes: intramuscular, intradermal and intranasal. Our studies in a mouse model show that the immunogenicity of our four different saRNA vaccine formulations after intramuscular or intradermal administration was initially comparable; however, ionizable LNPs gave higher long-term IgG responses. The clearance of all 4 of the nanoparticle formulations from the intramuscular or intradermal administration site was similar. In contrast, immune responses generated after intranasal were low and coupled with rapid clearance for the administration site, irrespective of the formulation. These results demonstrate that both the administration route and delivery system format dictate self-amplifying RNA vaccine efficacy.
Wednesday 15 June 2022
1:10 – 1:40 pm
The effect of sex & the tumor microenvironment on liposomal cancer treatments
Medicine is taking its first steps towards patient-specific cancer care. Nanoparticles have many potential benefits for treating cancer, including the ability to transport complex molecular cargoes including siRNA and protein, as well as targeting to specific cell populations.
The talk will discuss ‘barcoded nanoparticles’ that target sites of cancer where they perform a programmed therapeutic task. Specifically, liposomes that diagnose the tumor and metastasis for their sensitivity to different medications, providing patient-specific drug activity information that can be used to improve the medication choice.
The talk will also describe how liposomes can be used for degrading the pancreatic stroma to allow subsequent drug penetration into pancreatic adenocarcinoma, and how nanoparticle’ biodistribution and anti-cancer efficacy is impacted by patient’ sex and more specifically, the menstrual cycle.
The evolution of drug delivery systems into synthetic cells, programmed nanoparticles that have an autonomous capacity to synthesize diagnostic and therapeutic proteins inside the body, and their promise for treating cancer and immunotherapy, will be discussed.
Wednesday 15 June 2022
1:40 – 2:10 pm
Liposomal Antibiotics Induce Anticancer Immunity by Killing the Tumor-Associated Bacteria
The success of neoantigen cancer vaccine is mostly seen in tumor types with relatively high mutation burden. Neoantigens are rarely found in most of human cancers. On the other hand, many human solid tumors contain abundant intracellular bacteria. We hypothesized that the tumor associated bacteria (TAB) can be the best source for neoantigen if the bacterial antigen can be presented by the tumor cell’s antigen presenting mechanism. Mice bearing orthotopic colorectal cancer CT26 were infected by oral gavage of Fusobacteria nucleatum (Fuso). The bacteria could cross the gut epithelium and establish intracellular colonization in the tumor, which caused rapid growth and metastasis of the tumor cells. We have prepared liposomes containing two different antibiotics by the method of active loading. Intravenous injections of liposomal antibiotics effectively killed Fuso in the tumor, but did not affect the gut microbiome population. The death of Fuso triggered a strong T-cell mediated immunity against both infected and uninfected tumor cells which eradicated the tumor in the gut and in the liver metastasis. We hypothesized that strong bacteria epitopes that are shared by the host proteins are the major neoantigens recognized by the host immune system. Using tools of bioinformatics, we have predicted several such epitopes for testing. Synthetic peptides with the predicted sequence could be recognized by the tumor infiltrating T-cells as shown by using a tetramer assay. Thus, targeting TAB for immune recognition might be an alternative and effective approach as a cancer vaccine. Supported by NIH grant CA198999 and Fred Eshelman Distinguished Professorship.
Wednesday 15 June 2022
2:10 – 2:40 pm
On the structural characterization of lipid nanoparticle formulations of nucleic acid
Lipid nanoparticles containing short interfering RNA (LNP-siRNA) and optimized ionizable cationic lipids are now clinically validated systems for silencing disease-causing genes in hepatocytes following intravenous administration. However, the mechanism of formation and certain structural features of LNP-siRNA remain obscure. These systems are formed from lipid mixtures (cationic lipid, distearoylphosphatidylcholine, cholesterol, and PEG-lipid) dissolved in ethanol that is rapidly mixed with siRNA in aqueous buffer at pH 4 where the ionizable lipid is positively charged. The resulting dispersion is then dialyzed against a normal saline buffer to remove residual ethanol and raise the pH to 7.4 (above the pKa of the cationic lipid) to produce the finished LNP-siRNA systems. Here we provide cryogenic transmission electron microscopy and X-ray evidence that the complexes formed between siRNA and ionizable lipid at pH 4 correspond to tightly packed bilayer structures with siRNA sandwiched between closely apposed monolayers. Further, it was shown that ionizable lipid not complexed to siRNA promotes formation of very small vesicular structures at pH 4 that coalesce to form larger LNP structures with amorphous electron dense cores at pH 7.4. A mechanism of formation of LNP-siRNA systems is proposed whereby siRNA is first sandwiched between closely apposed lipid monolayers at pH 4 and subsequently trapped in these structures as the pH is raised to 7.4, whereas ionizable lipid not interacting with siRNA moves from bilayer structure to adopt an amorphous oil phase located in the center of the LNP as the pH is raised.